I. What is the Composition and Function of Blood?
If we can continue the highway transport analogy in regards to describing the cardiovascular system, the blood is best thought of as the mail/delivery carriers! Blood allows for the carrying and delivery of oxygen, various nutrients, cells, etc. throughout the body to ensure proper function, hopefully, more efficiently than UPS or FedEx (sorry about the shade….).
While it’s hard to have favoritism in regards to picking which component of the cardiovascular, you can argue that blood has to be right up there due to the various functions it has! Let’s go ahead and give you all a better understanding of blood and its importance in cardiovascular physiological function.
II. Composition and Function of Blood
We’ll try to keep our covering of the different structural components of the cardiovascular and lymphatic system to the main components without going too deep in detail in regards to the more specific histology and anatomy of these structures.
Rather, we’ll keep our focus and discussion to the major, high yield breakdown of the systems with a bigger emphasis on their physiological applications!
A. Composition
Blood can be divided into 2 different components: cellular and plasma components. As the name implies, the cellular components contain the cells that travel within the blood while the plasma is the actual liquid component.
I. Cellular
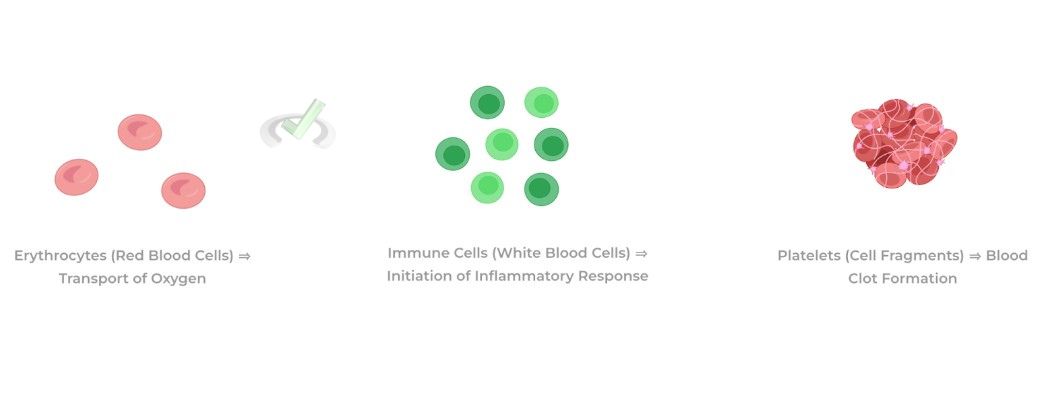
The main cells present within the blood are erythrocytes (red blood cells), immune cells (white blood cells), and platelets. Without getting too much into the details of their functions, erythrocytes allow for transport of oxygen throughout the body to be delivered throughout the body.
Immune cells circulate throughout the body and are ready to enter into tissues where infection is present. Finally, platelets are actually cell fragments which allow for the formation of clots in order to prevent bleeding.
II. Plasma
This is the actual liquid component of blood and has many molecules dissolved which are also transported throughout the body. These include ions such as sodium, chloride, and calcium which act as important electrolytes throughout the body.
Additionally, plasma also contains important proteins such as albumin which acts as to both maintain blood vessel oncotic pressure as well as a transport protein for hydrophobic molecules (i.e. steroid hormones in endocrine signaling)
B. Function
A majority of our discussion regarding the function of blood will focus on the erythrocytes (red blood cells) because of their importance in regards to transporting oxygen throughout the body! Additionally, we have a more extensive covering of the various immune cells in our immunology division of our study notes!
I. Transport of Oxygen via RBCs and Hemoglobin
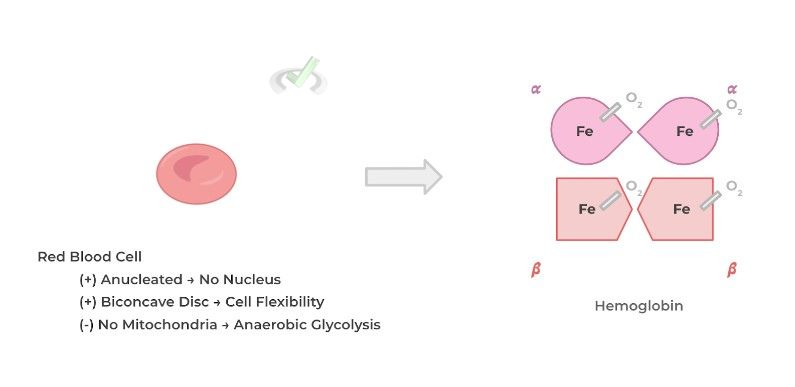
As mentioned, oxygen is delivered throughout the body via the erythrocytes because they have an important oxygen carrying protein called hemoglobin. In order to maximize the amount of oxygen to be transported, RBCs lose most of their intracellular organelles during their development!
As such, erythrocytes are devoid of a nucleus, mitochondria, ribosomes, etc. which allows more space to be occupied by hemoglobin. Additionally, the lack of a mitochondria results in the RBCs generating ATP via anaerobic glycolysis!
A hemoglobin protein is actually composed of 4 protein subunits: 2 alpha and 2 beta subunits. Each of these subunits has a heme group (a type of prosthetic group) with a central iron atom — it’s this central iron atom that allows for the binding of oxygen. Multiply this by 2
An important concept in regards to the binding affinity of hemoglobin to oxygen is the concept of cooperative binding. In its simplest sense, cooperative binding refers to how the binding of one heme subunit to oxygen increases the affinity/likelihood the other heme group will bind to another oxygen atom!
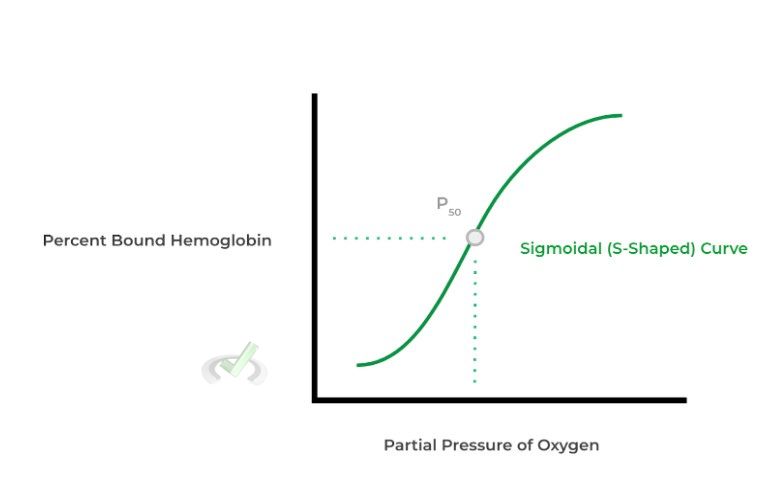
Because of cooperative binding, when we plot the partial pressure of oxygen against the percent of hemoglobin bound, we see that the line that emerges follows a sigmoidal pattern — this curve is called the oxygen dissociation curve and is a visual depiction of cooperative binding!
Note that instead of a linear increase in percent of bound hemoglobin, note that in the sigmoidal curve there’s a sharp increase in the percent of hemoglobin bound which is due to the effect of cooperative binding! Note also the value below called P50: this is the partial pressure of oxygen at which 50% of the hemoglobin is saturated/bound to oxygen.
A very important concept to understand in regards to the oxygen dissociation curve are right and leftward shifts that occur for the curves and the various conditions that can cause these shifts. Before understanding what conditions can cause these shifts, it’s important to first understand what the shifts indicate:
- A rightward shift indicates that the hemoglobin’s affinity for oxygen is DECREASED — this is because by shifting the curve to the right, it takes a higher partial pressure of oxygen for 50% of the hemoglobin to be bound (i.e. a higher P50).
- A leftward shift indicates that the hemoglobin's affinity for oxygen is INCREASED — this is because by shifting the curve to the left, it takes a lower partial pressure of oxygen for 50% of the hemoglobin to be bound (i.e. a lower P50).
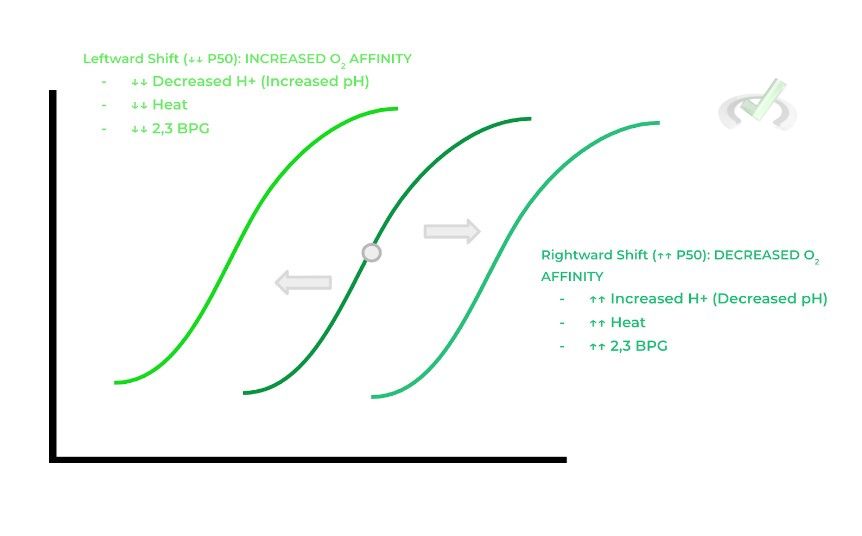
Notice anything about the conditions that cause a rightward shift? They primarily indicate conditions or states where tissue metabolism is actively occurring! This explains why there would be a rightward shift: this would result in decreased oxygen affinity and allows for more oxygen to be unloaded to the tissue which can be used for metabolism!
II. CO2 Transport and The Bicarbonate Buffer System
Arguably, the most important function of the plasma component of blood is to also allow for the transport of carbon dioxide. Recall that carbon dioxide is a metabolic byproduct of oxidative phosphorylation and must be properly disposed via the respiratory system.
It’s important to note that because carbon dioxide is nonpolar, it has poor solubility in plasma — as a result, a majority of carbon dioxide is transported in the form of bicarbonate (HCO3-). This is accomplished via a clever set of chemical reactions as shown below:
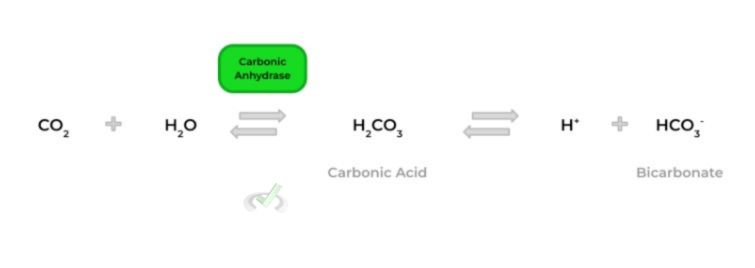
As shown above, carbon dioxide can combine with water to allow for the formation of carbonic acid catalyzed by the enzyme carbonic anhydrase. Carbonic acid then subsequently dissolves into protons (H+) and bicarbonate, which can then travel from systemic tissue and enter into pulmonary circulation.
Once at pulmonary circulation, the reverse reaction occurs which regenerates carbon dioxide which can be exhaled! Additionally, the presence of bicarbonate within the bloodstream also allows for a buffering system to be present!
Because bicarbonate is a base, it can react within incoming acids and neutralize them in order to prevent any major blood pH changes. Think about this importance physiologically: many enzymes require a specific pH range to function properly and any alterations in these pH levels can result in dysfunctional enzymes.
III. Erythrocyte Surface Antigens
Finally, it’s important to touch upon the importance of various surface antigens present on the red blood cells, particularly the ABO and Rhesus Factor (Rh) antigens. These antigens do have important structural and functional roles but are best examined through the lens of immunoreactivity and blood transfusions.
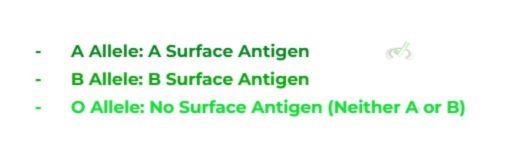
Let’s first begin with the ABO as it’s a little more complex: that we have 2 alleles for a specific gene due to the paired chromosomes. For the ABO gene, there are 3 alleles present which are expressed in a codominant fashion:
Recall that in codominance, both alleles will be expressed as all alleles technically display a dominant pattern (i.e. only one allele needs to be present in order to express the phenotype). Here’s what they would look like below and the possible associated genotypes.
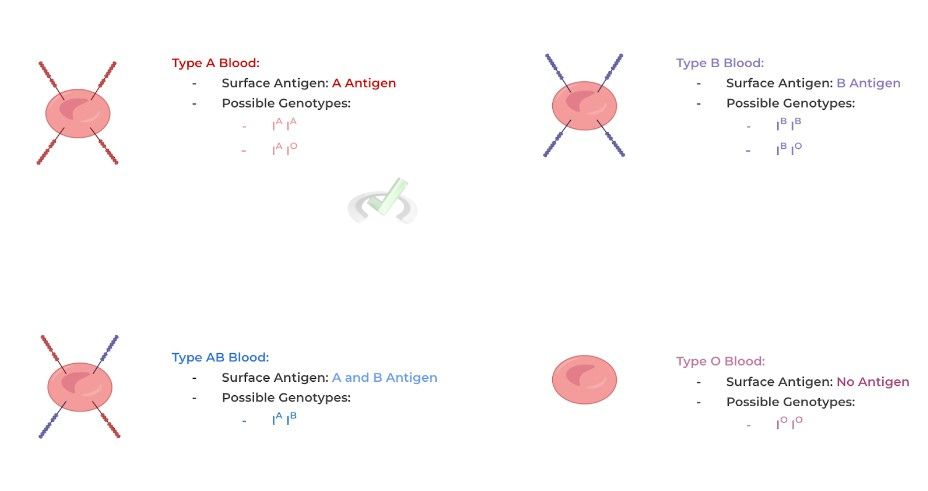
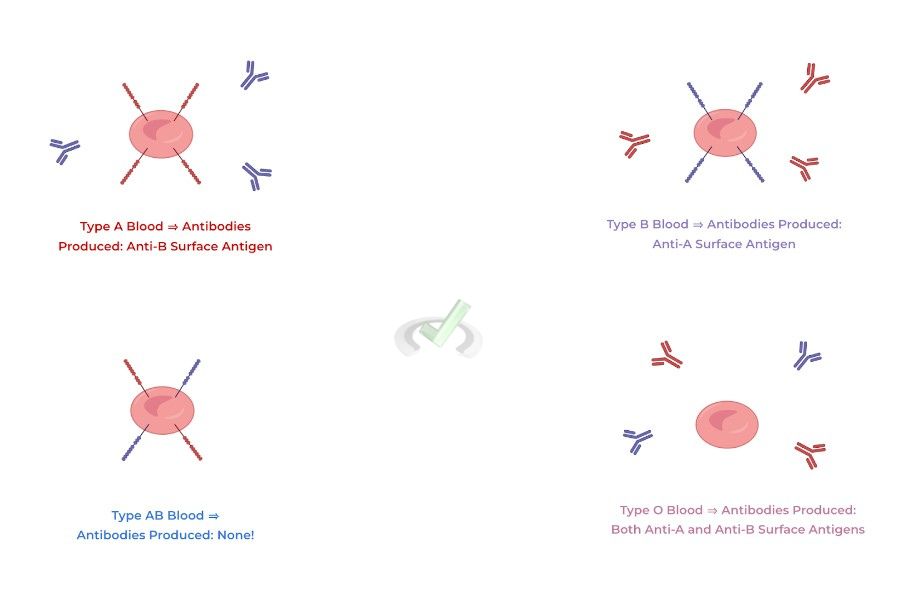
Finally, it’s important to note that the different blood types will have different antibodies produced depending on what surface antigen is present on the red blood cell. This is important when cross referencing recipient and donor blood for a transfusion in order to prevent an immunoreaction!
If there’s a mismatch in regards to the recipient's RBC antigens and the donor antibodies (or vice versa), the donor antibodies can attack the recipient RBC surface antigens resulting in a possibly life threatening transfusion reaction! We can deduce the antibodies present in a specific blood type via the following statements:
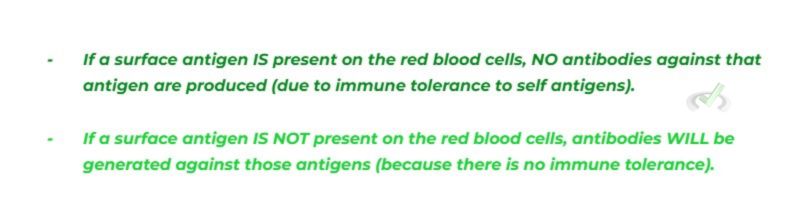
Now following these statements, see if the following diagram below makes sense!
The Rhesus Factor (Rh) basically works the same way except that there’s only 2 alleles present: a Rh (+) allele which codes for the Rh surface antigen and the Rh (-) allele which results in no Rh surface antigen being present. In addition, instead of being a codominant pattern, the Rh factor follows an autosomal recessive pattern where 2 Rh (-) alleles are needed to express no Rh surface antigen.
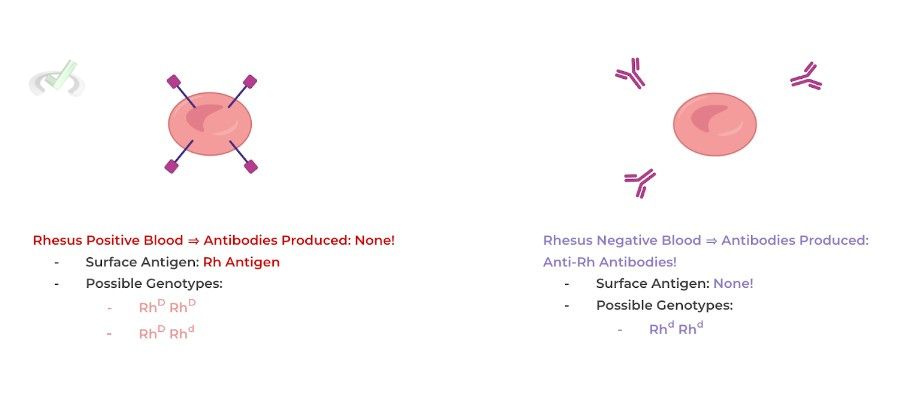
From here, we can understand why O negative (type O blood that’s Rhesus-negative) is called the universal donor and why AB+ (type AB blood that’s Rhesus-positive) is called the universal acceptor when it comes to blood transfusions.
O negative blood contains no antigens that can react with a recipient’s serum and cause an immune reaction, meaning that it can be given to individuals of all blood types. Conversely, AB positive blood types can receive from all blood types because they lack any antibodies within their serum which can similarly cause a reaction to the donor RBCs.
III. Bridge/Overlap
The bicarbonate buffer system is actually the basis of what is physiologically disturbed when the body enters into an acidotic state (i.e. blood pH becomes too low) or an alkalotic state (i.e. blood pH becomes too high). To understand this, let’s review the concepts of Le Chatelier’s Principle.
I. Le Chatelier’s Principle
Recall that Le Chatelier’s principle states that when there is a change in the equilibrium state of a system, there will be a shift in equilibrium in order to offset that change.
In this case for the bicarbonate buffer system, increasing the concentration of CO₂ would shift the equilibrium to the right. In order to return to our original position, we would need to increase the concentration of H⁺ in order to restore equilibrium.
This would be a great example of respiratory acidosis due to hypoventilation: when you hypoventilating, you’re not exhaling as much which results in an increased buildup of CO2 within the blood!

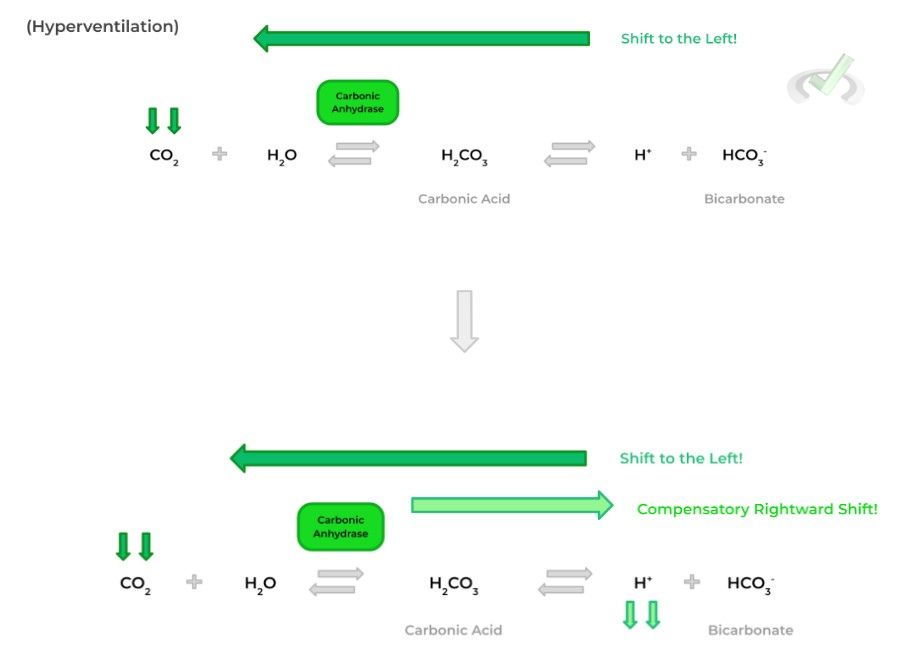
Conversely, if our CO₂ concentration decreased, this would shift our equilibrium to the left. Likewise, in order to return the equilibrium to the original position, we’d have to decrease the concentration of H⁺ in order to restore equilibrium.
In this case, respiratory alkalosis would occur due to hyperventilation: when you hyperventilate, you exhale too much which results in a decrease in CO2 within the bloodstream.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Composition
Blood can be divided in 2 main constituents: the cellular component (which as the name implies contains all the cells which travel within blood) and the plasma component (which is the actual liquid component of blood).
I. Cellular
The main cells that compose the cellular component include erythrocytes (red blood cells), immune cells (white blood cells), and platelets (which are technically cell fragments).
II. Plasma
Due to it being the liquid component, plasma has many substances dissolved in it including various ions which act as electrolytes and various plasma proteins such as albumin which has many functions including maintaining oncotic pressure and transporting nonpolar substances.
B. Function
The main function of blood is to allow for the transport of gasses and nutrients throughout the body. Blood also has many other functions including trigger clotting to prevent the loss of blood, maintaining a normal physiological pH range, etc.
I. Transport of Oxygen via RBCs and Hemoglobin
The transport of oxygen is accomplished through red blood cells because of the presence of hemoglobin, an oxygen carrying protein. A hemoglobin protein is composed of 4 protein subunits, each with a heme group which allows for the binding of oxygen via a central iron atom.
Binding of oxygen to hemoglobin occurs via cooperative binding, meaning that the binding of one oxygen atom to one heme group increases the likelihood that another heme group can bind to another oxygen atom — this is shown via a sigmoidal (S) line on the oxygen dissociation curve.
The oxygen dissociation curve can experience left and rightward shifts which indicate increase and decrease oxygen affinity, respectively. Generally speaking, conditions which indicate an active metabolic state such as increased temperature, increased 2,3 BPG, and decreased pH will cause a rightward shift!
II. CO₂ Transport and The Bicarbonate Buffer System
It’s important to note that a majority of carbon dioxide is transported in the blood as bicarbonate in order to be properly exhaled at the lung! This is accomplished via a set of chemical reactions which allows for the conversion of carbon dioxide into bicarbonate.
The presence of bicarbonate also allows for a buffering system to be present — should any additional acids be added, the bicarbonate can react with the incoming acids and neutralize them to maintain a narrow physiological pH range!
III. Erythrocyte Surface Antigens
Finally, there are various RBC surface antigens present on the red blood cells which are important when considering blood transfusions and transfusion reactions! The main surface antigens that are the ABO and Rhesus factor surface antigens!
The ABO antigens are inherited in a codominant pattern: the A allele codes for the A surface antigen, the B allele codes for the B surface antigen, and the O allele codes for no antigen. The Rhesus factor (Rh) is inherited in an autosomal recessive pattern where it takes two Rh (-) alleles to result in no expression of the Rh surface antigen.
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
In erythrocyte metabolism, which of the following would you expect to be in abundance compared to a normal cell?
A. Lactic Acid
B. DNA Replication Enzymes
C. Citric Acid Cycle Enzymes
D. Acetyl-CoA
Ans. A
Recall that because of the lack of mitochondria, red blood cells must partake in anaerobic glycolysis in order to produce ATP. This results in an increase in lactic acid due to lactic acid fermentation.
Sample Practice Question 2
A person is found to have a A Positive (+) blood type. Which of the following blood types can be given to the patient during a blood transfusion?
I. O Negative (-)
II. O Positive (+)
III. A Negative (-)
A. I only
B. I and II
C. II and III
D. I, II, and III
Ans. D
A person who is A Positive (+) will only have anti-B antibodies within the serum because it will have self tolerance to the A surface antigens and the Rhesus factor (Rh) antigen.


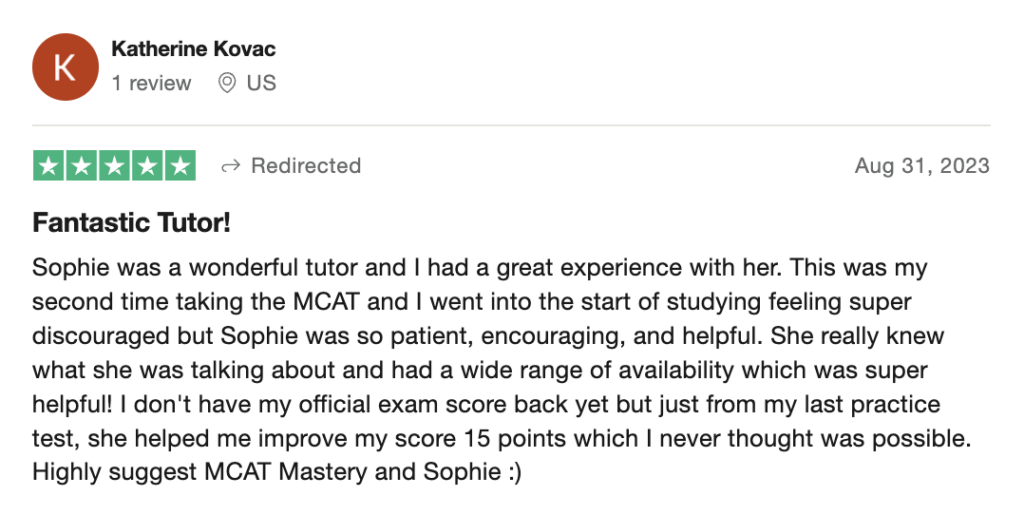
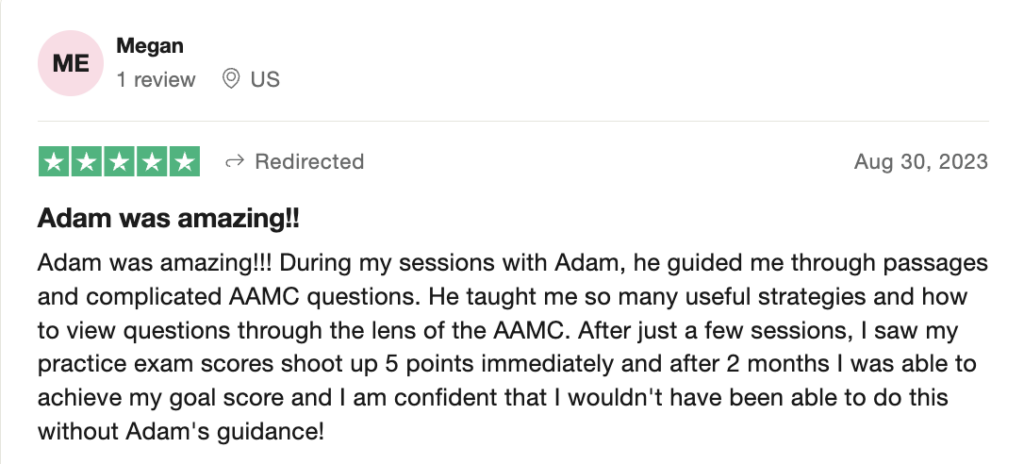
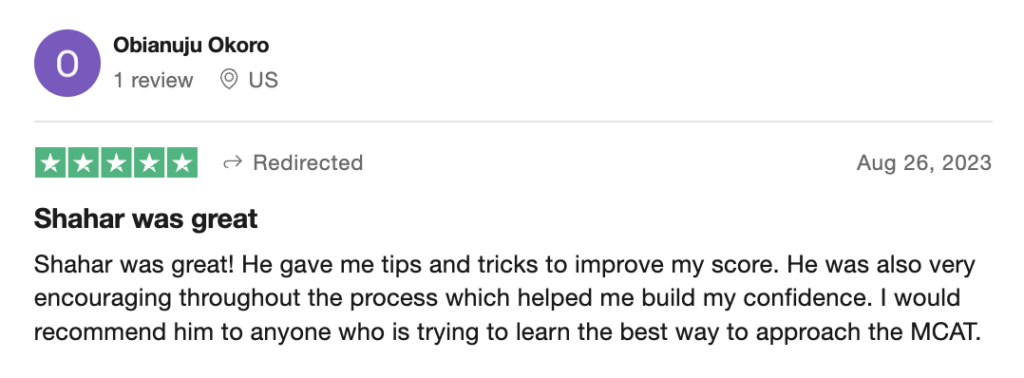
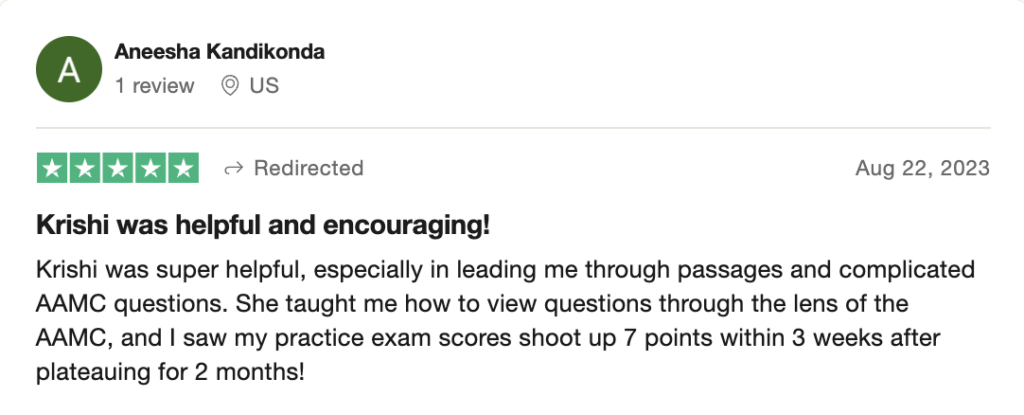
 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these