I. What is the Neuroendocrine Control of the Cardiovascular System?
While we all can appreciate the cardiovascular system’s main function in circulating blood, nutrients, and oxygen throughout the body, it’s equally as important to note that regulation of this system and its function is not just independent, but is carefully intertwined with the nervous and endocrine system.
The literal feeling of your “blood pumping” and “heart racing” when you’re exercising or you’re on a rollercoaster is a result of the interplay between the nervous and endocrine system with the cardiovascular system. Let’s take a look at this interplay and how crosstalk between these systems can allow for our body to maintain homeostasis and quickly adapt to situations!
II. Neuroendocrine Control of the Cardiovascular System
Let’s first break down the term neuroendocrine: the “neuro” component refers to the nervous system — particularly how the nervous system integrates incoming afferent sensory stimuli and sends the appropriate efferent signals to various organs to initiate the appropriate cardiovascular response.
In certain cases, as we’ll see in the sympathetic v.s. parasympathetic response, the efferent signals from the nervous system stimulate endocrine organs which result in the release of endocrine hormones into the bloodstream to initiate the cardiovascular response — this comprises the “endocrine” component. Note, however, that there are times when the systems work independently from one another as we’ll see in a bit.
A. Sympathetic v.s. Parasympathetic Response
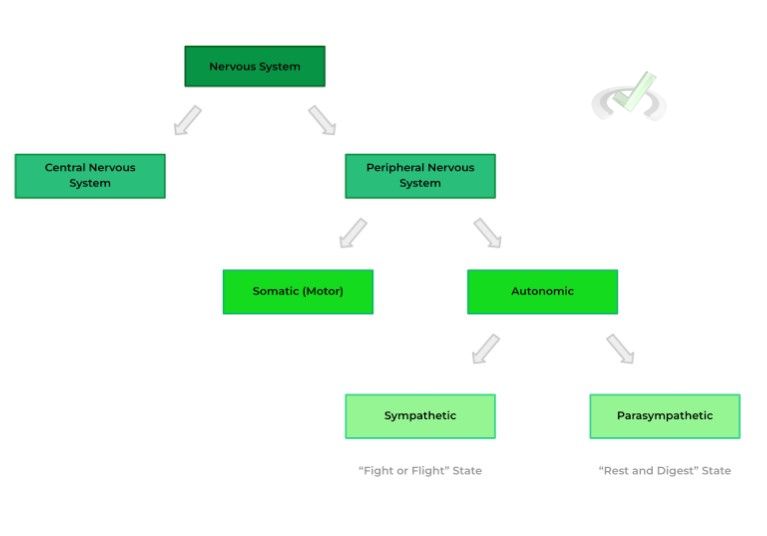
If you’ve covered some basic behavioral sciences or psychology, you may be familiar with these terms! In its simplest terms, your sympathetic response is your nervous system response in situations of high stress, also abbreviated as your “fight or flight” response.
Conversely, your parasympathetic response occurs in situations where the body is going about daily function without stress, also abbreviated as your “rest and digest '' response. Recall also that the sympathetic and parasympathetic nervous systems are a subdivision of the autonomic nervous system.
I. Sympathetic Response
When picturing a scenario where the sympathetic response is active, imagine yourself being chased by a lion or tiger in the middle of the jungle. Now unless you’re some alpha or just built different to fight, you’ll most likely be running as fast as you can in the opposite direction.
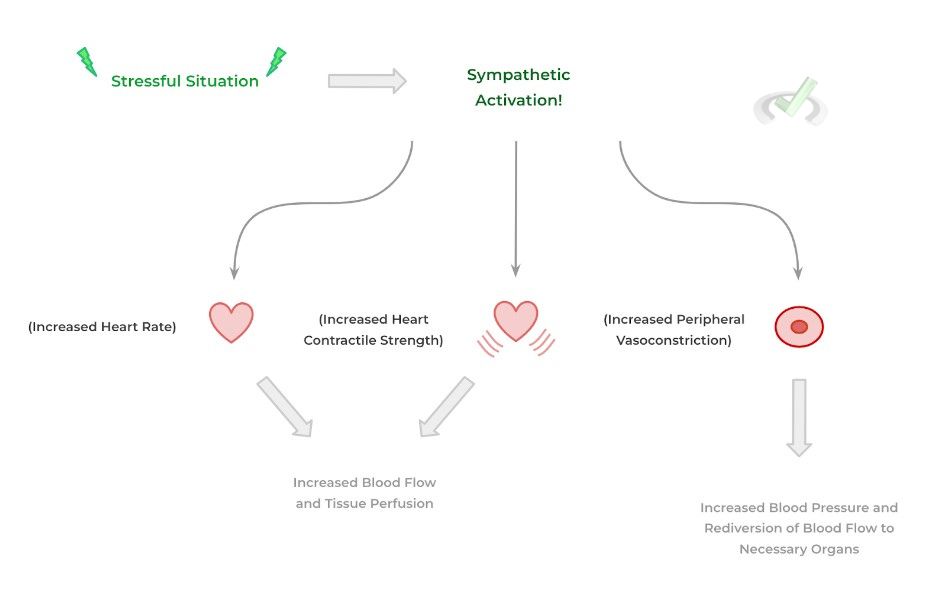
When the nervous system recognizes that the individual is in a scenario of stress, the sympathetic system is activated and will primarily result in 3 main cardiovascular physiological changes as shown below:
- Increased Heart Rate (i.e. Positive Chronotropy)
- Increased Heart Contractile Force (i.e. Positive Inotropy)
- Increased Peripheral Vasoconstriction (i.e. Decreased Vascular Diameter)
The actions of the SNS is mediated by the neurotransmitters/endocrine hormones called norepinephrine (NE) and epinephrine (E) — these molecules bind to adrenergic receptors located within the heart and vascular smooth muscle and trigger a signal cascade which eventually results in the above mentioned cardiovascular changes.
These molecules can be released in 2 main ways: 1) via nerve endings of postganglionic sympathetic fibers and 2) via the adrenal gland (specifically, the adrenal medulla). Their release via nerve fibers can be thought of as “endocrine independent” while their release via the adrenal gland is best termed a “neuroendocrine” mediated release.
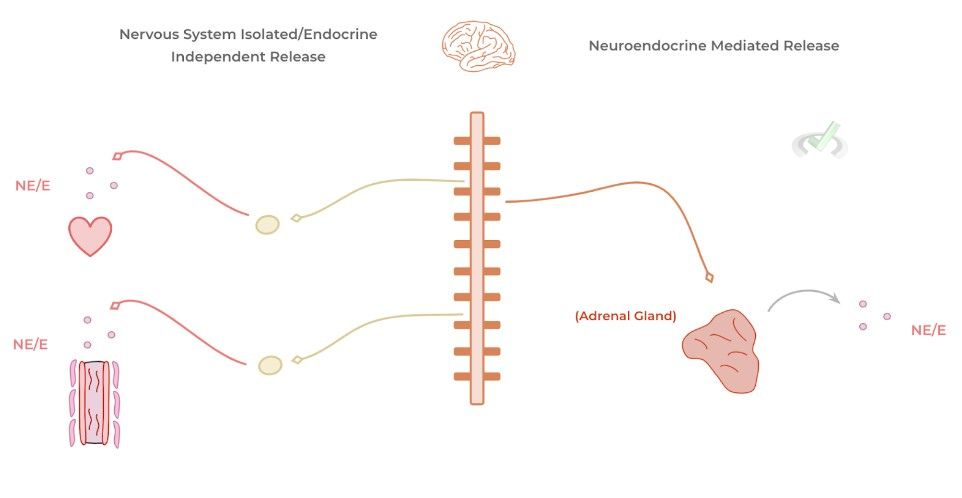
Though both mechanisms result in the release of NE/E, there are specific characteristics for each pathway in regards to their range of action and duration. The pathway involving via nerve endings allows for an immediate initiation of the sympathetic pathway but more limited in regards to which organs they can act upon.
The initiation of sympathetic cardiovascular changes via neuroendocrine release by the adrenal gland is a bit slower due to the time it takes for the released endocrine hormones to enter into the bloodstream and be carried systematically — however, because of their travel within the bloodstream, they have a wider range of action!
II. Parasympathetic Response
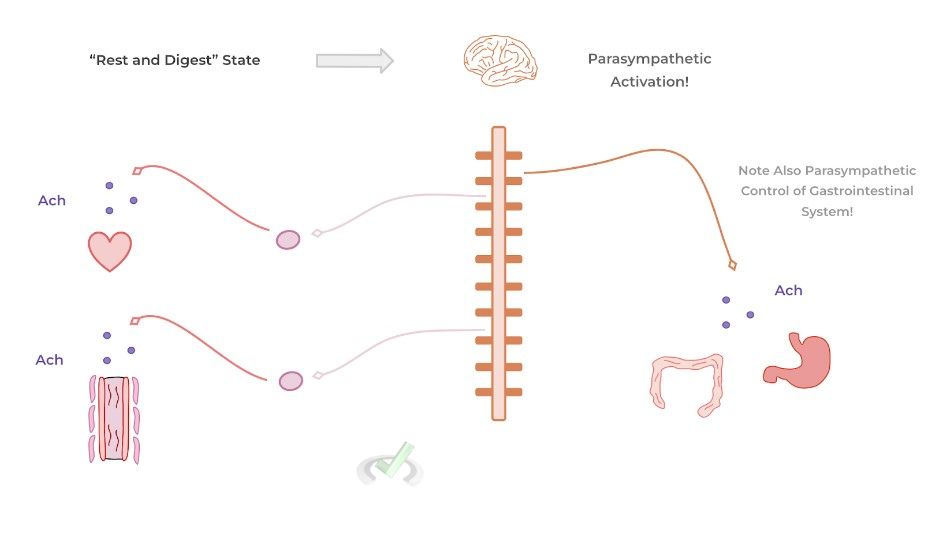
The great thing when it comes to learning the cardiovascular changes for the parasympathetic response, it’s basically just the opposite of those we talked about for the sympathetic response!
- Decreased Heart Rate (i.e. Negative Chronotropy)
- Decreased Heart Contractile Force (i.e. Negative Inotropy)
- Increased Peripheral Vasodilation (i.e. Increased Vascular Diameter)
Similarly, if we think about the purpose of the parasympathetic response, we can easily understand why the above mentioned cardiovascular changes occur! Because the body isn’t in a state of stress and is simply going about its daily function, there’s no critical need for blood flow to meet energy requirements.
In contrast to the sympathetic nervous system, the main neurotransmitter that initiates parasympathetic physiological changes is acetylcholine which binds to muscarinic receptors of target organs.
In addition, the release of acetylcholine is primarily restricted to the nervous system and is only released via nerve ending of parasympathetic fibers. There’s no systemic, endocrine release of acetylcholine though it makes up for this by having a widespread amount of parasympathetic fibers.
B. Effects of the RAAS System and Antidiuretic Hormone
Let’s go ahead and talk about some of the main contributions of various endocrine signaling pathways and their contributions to their control on the cardiovascular system. We’ll mainly focus on the RAAS system (specifically, the effects of angiotensin II and aldosterone) and antidiuretic hormone (a.k.a. vasopressin).
I. RAAS System
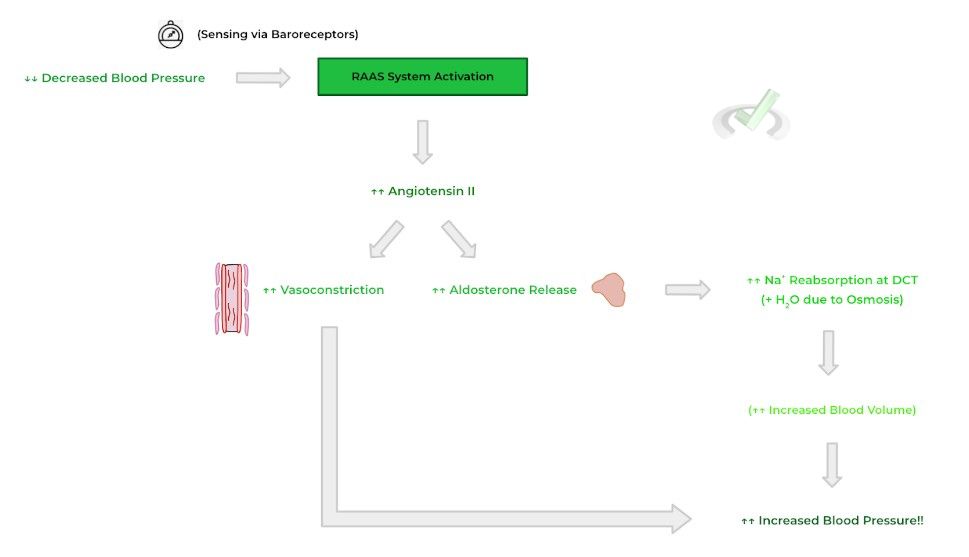
Recall that the RAAS system stands for the renin-angiotensin-aldosterone system and that the main goal of the RAAS system is to increase blood volume which leads to a concurrent increase in blood pressure. As such, the main stimulus which triggers the activation of the RAAS system is decreased blood pressure sensed by renal baroreceptors.
The 2 most important molecules which are released upon RAAS activation are angiotensin II and aldosterone. When bound to receptors, angiotensin II results in peripheral vascular smooth muscle contraction and vasoconstriction in order to increase blood pressure.
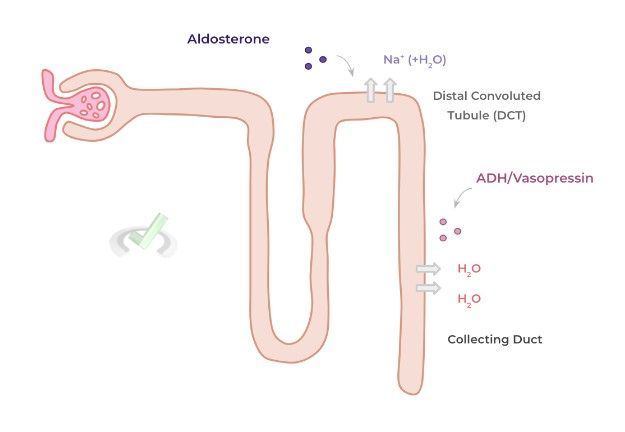
Additionally, angiotensin II allows for the release of aldosterone by the adrenal cortex! Aldosterone acts on receptors for the tubular renal cells at the distal convoluted tubule to promote sodium reabsorption into the bloodstream — water than follows the reabsorbed Na+ back into the bloodstream via osmosis resulting in an increase in blood volume and a concurrent increase in blood pressure!
II. Antidiuretic Hormone
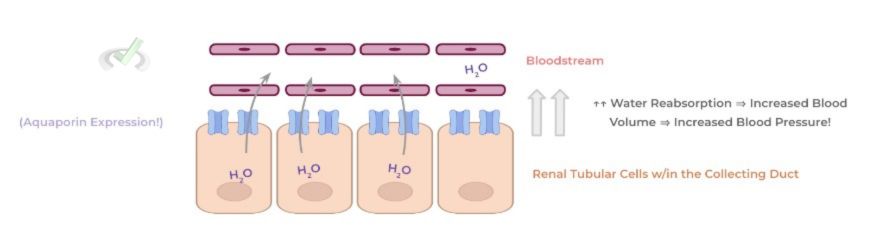
ADH/vasopressin is a hormone that’s also released in response to low blood pressure and released by the posterior pituitary gland. The mechanism of action of ADH is much simpler: upon release, ADH binds to receptors located in the collecting duct of the kidney.
Binding of ADH triggers the increased expression of aquaporins on the basal surface of the renal tubular cells which promotes increased water reabsorption, resulting in an increased blood volume and a concurrent increase in blood pressure!
Finally, take a look at a comprehensive diagram below for a simple and quick summation of the 2 hormones and their physiological effects on the renal and cardiovascular system.
III. Bridge/Overlap
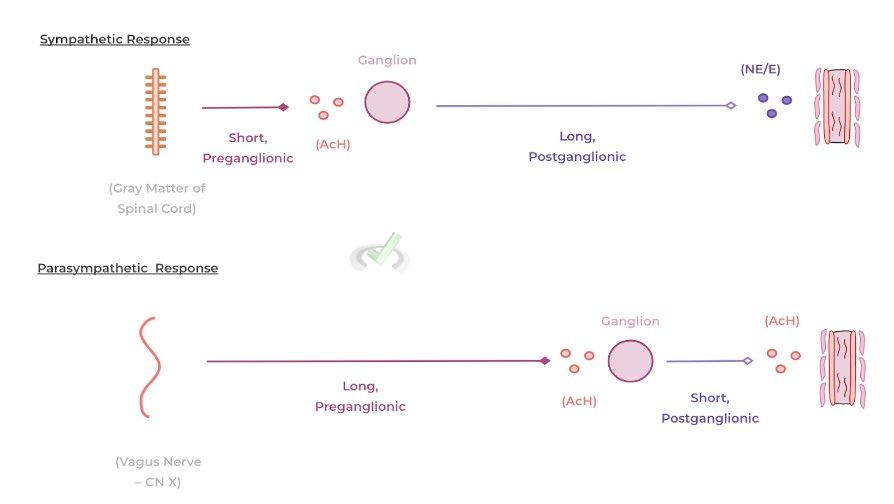
As we mentioned, the neurotransmitters/hormones of the sympathetic and parasympathetic nervous systems can be released via post ganglionic nerve endings to enact their respective functions. As such, it may be beneficial to have a recap of how these nerve fibers are organized in order to relay signals!
I. Pre and Postganglionic Nerve Fiber Organization
The main structure that’s critical in connecting efferent signals from the central nervous system to the peripheral nervous system is the ganglion. These are simply collections of cells which act as a relay station for incoming signals from the CNS and relays those signals to the peripheral effector organs and tissues!
From the spinal cord, there are preganglionic fibers which extend and synapse on the ganglion. From here, the signals are integrated and extend from the ganglion via postganglionic fibers which then synapse onto effector organs and release neurotransmitters to enact their function.
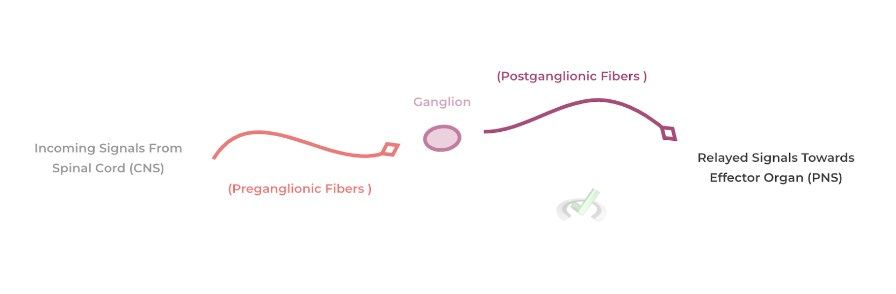
Both the sympathetic and parasympathetic nerve endings communicate in this sense, but they have distinct similarities and differences in regards to the length of the various preganglionic and postganglionic nerve fibers, the neurotransmitters involved, and the origin of the CNS signals.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Sympathetic v.s. Parasympathetic Response
The sympathetic and parasympathetic nervous systems are subdivisions of the autonomic nervous system. In short, your sympathetic nervous system is termed your “flight or fight” response while your parasympathetic response is termed your “rest and digest” response.
I. Sympathetic Response
There are 3 main cardiovascular responses that occur upon activation of the sympathetic nervous system: 1) increase in heart rate, 2) increase in heart contraction, and 3) increase in peripheral vasoconstriction.
An increase in heart rate and contraction allows for increase blood flow and perfusion to tissues in high metabolic demand. Additionally, peripheral vasoconstriction (particularly, at the skin) allows for diversion of blood flow to tissue in more important organs such as the heart and skeletal muscles.
The main neurotransmitter/hormone for the sympathetic response is epinephrine and norpeinphrine which binds onto adrenergic receptors and can either be released from post-ganglionic sympathetic nerve fibers or the adrenal gland, specifically at the adrenal medulla.
II. Parasympathetic Response
Conversely, the main cardiovascular changes of the parasympathetic response simply oppose those of the sympathetic response: 1) decrease in heart rate, 2) decrase in heart contraction, and 3) increase in peripheral vasodilation.
For the parasympathetic response, the main neurotransmitter which initiates this resposne in acteylcholine which bind to muscarinic receptors and unlike the sympathetic nervous system response, is only released in post-gangiolinc parasympathetic nerve fibers.
B. Effects of RAAS System and the Antidiuretic Hormone
Both of these systems respond to a decrease in blood pressure which is sensed by baroreceptors located throughout the body, but particulary at the renal tubular cells of the kidney.
I. RAAS System
The RAAS system is also called the renin-angiotensin-aldosterone system which works to increase blood pressure. The release of angiotensin II results in vasoconstriction and the release of aldosterone from the adrenal cortex.
Aldosterone can then bind to renal tubular cells located within the distal convoluted tubules of the kidney to allow for sodium reabsorption — this also allows for water reabsorption due to osmosis which increases blood volume and thus increases blood pressure.
II. Anti-Diuretic Hormone
Also called vasopressin, ADH is released by the posterior pituitary gland in response to decreased blood pressure. ADH then binds to respective receptors located in the collecting duct resulting in the increase expression of aquaporins. This allows for the reabsorption of water which increase blood volume and thus increase blood pressure.
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
Propanol is a type of beta-blocker medication often given in cases of tachycardia which binds to adrenergic receptors to prevent their binding to their normal signaling molecules. What would be one of the main effects of these medications?
A. Increased Heart Rate
B. Decreased Heart Rate
C. Increased Vasoconstriction
D. Increased Heart Contractility
Ans. B
Because beta-blockers block the effects of norepineprhine and epinephrine by blocking their binding to adrenergic receptors and decreasing sympathetic activation. As such, heart rate decreases due to lack of sympathetic innervation.
Sample Practice Question 2
Syndrome of Inappropriate Anti-Diuretic Hormone release (SIADH) is a condition where there is an excessive release of ADH with no negative feedback activated to suppress its release. Which of the following physiological changes would you expect to occur in this condition?
A. Hyponatremia (Decreased Salt Osmolarity)
B. Hypernatremia (Increased Salt Osmolarity)
C. Decreased Blood Pressure
D. Decreased Blood Volume
Ans. A
An increase of ADH release would result in a significant increase in water reabsoprtion into the bloodstream. This increase reabsoprtion of water dilites the bloodstream and results in DECREASED osmoloarity (i.e. solute concentration decreases). As such, hyponatremia occurs.



 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these 

 reviews on TrustPilot
reviews on TrustPilot