I. What is the Main Function and Structure of the Respiratory System?
When looking at practices such as yoga, taichi, and even something like karate (which on the surface looks aggressive and unlike the other 2 practices), they actually all have something in common: an emphasis on how one’s breath translates to one’s overall well being — both physically and spiritually!
Our mindful breathing and the benefits we can attain from such a practice is garnered by our respiratory system! In this article, let’s go ahead and examine the structures and main roles of this system which allows us to breathe and hopefully distress every once and a while!
II. General Principles of Respiratory System
In its most basic form, the main role of the respiratory system is gas exchange where O₂ rich inhaled air can be brought into the respiratory system to supply the body while the metabolic byproduct of CO₂ can be exhaled — the process of gas exchange occurs at the level of the alveoli which we’ll touch upon soon!
A. Upper and Lower Respiratory System
A great way to get accustomed to the different structures of the respiratory system is to divide it into an upper and lower portion — as we’ll see, the main dividing point between the 2 tracts is the epiglottis whose function we’ll examine in just a bit!
I. Upper Respiratory Tract
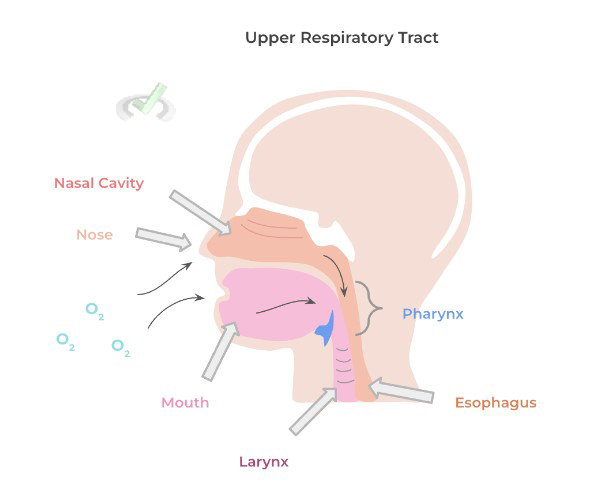
There are 4 main structures which constitute the upper respiratory tract (URT): the nose, nasal cavity, the mouth, and the pharynx. From the URT, air can flow in either from the nose into the nasal cavity or via the mouth.
In both cases, air eventually enters into the pharynx which is a muscular tube-like structure located behind the nasal cavity and mouth — the pharynx can lead into either the larynx which continues the respiratory tract or the esophagus continuing into the alimentary canal!
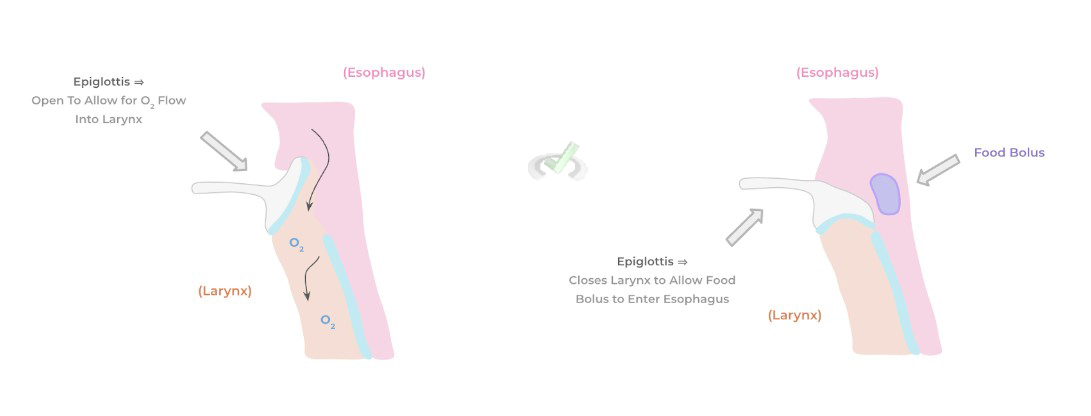
You may have also noticed that little blue structure located just on top of the larynx: this is the epiglottis, a structure composed of elastic cartilage which has another important role aside from being the divider between the upper and lower respiratory tract.
Because the pharynx leads both into the larynx and esophagus, the epiglottis ensures that food only enters into the esophagus and alimentary tract!
While eating, the esophagus covers the larynx so that food from the pharynx goes into the esophagus. Conversely, during normal breathing, the epiglottis is open so that air from the pharynx enters into the larynx which continues the respiratory tract!
II. Lower Respiratory Tract
Continuing from the epiglottis (again the main divider) is the larynx, also known as your voice box as it contains the vocal cords needed to produce sound. The larynx leads directly into the trachea also known as the windpipe and marks the beginning portion of the lung!
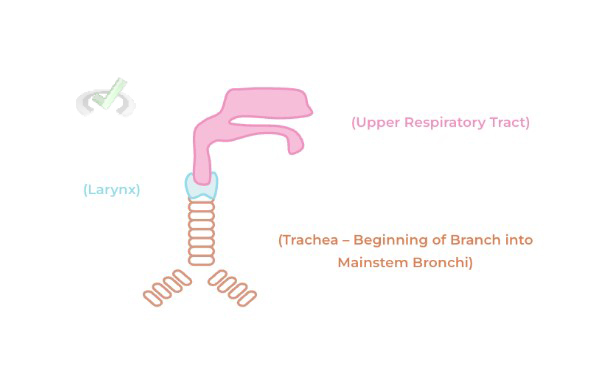
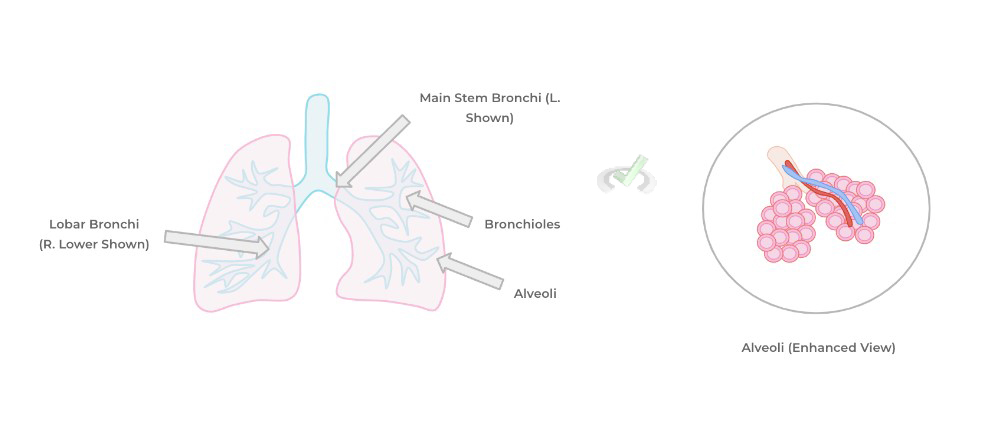
The trachea splits into 2 main stem bronchi: 1 right and 1 left main stem bronchus corresponding to the right and left lung! They then branch into what are called lobar bronchi, which correspond to the lobes of the right and left lung: 3 on the right and 2 on the left!
They then branch into smaller airway structures called bronchioles (similar to how arteries branch into arterioles!) and finally ending at the level of the alveoli which are sac-shaped structures where gas exchange takes place!
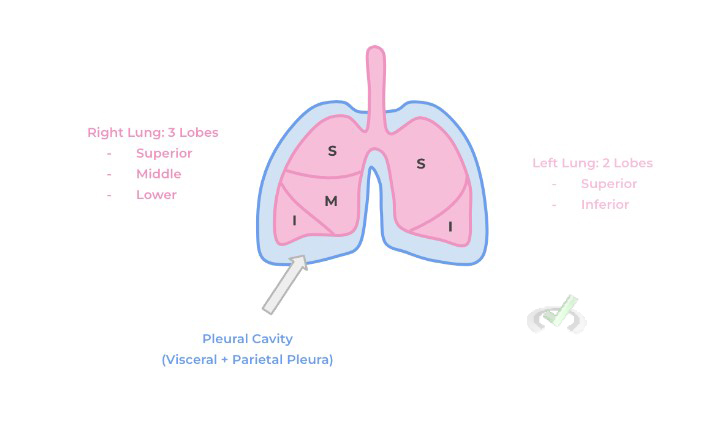
III. Lung Lobes and the Pleural Cavity
The right and left lung can be divided into different lobes: 3 on the right lung and 2 on the left. The right lung contains the superior, middle, and inferior lobe, separated by lines called fissures. The left lung only contains a superior and inferior lobe separated by 1 fissure.
Similar to the heart, the lungs are also encased by a sac called the pleural cavity — like the pericardial sac, the pleural cavity is also 2 membraned, lined structure with the visceral pleura lining the lung parenchyma and the parietal pleural lining the outside and function in protection and lubrication to allow for effective breathing.
B. Alveolar Structure and Gas Exchange
We’ll have to go a little more in depth in regards to the structure of the alveolar sac as they’re so important in regards to understanding the process of gas exchange! First, it’s key to note that the alveoli is structured as a duct outlined by a simple squamous epithelium as shown below:
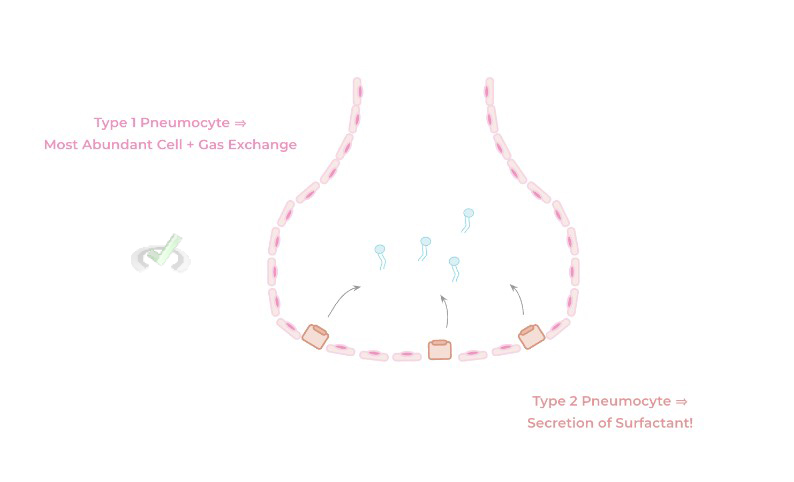
There are 2 types of cells that line the alveoli: type 1 and type 2 pneumocytes. type 1 pneumocytes are the most abundant cell, lining about 90% of the alveoli, and are the main cells participating in gas exchange.
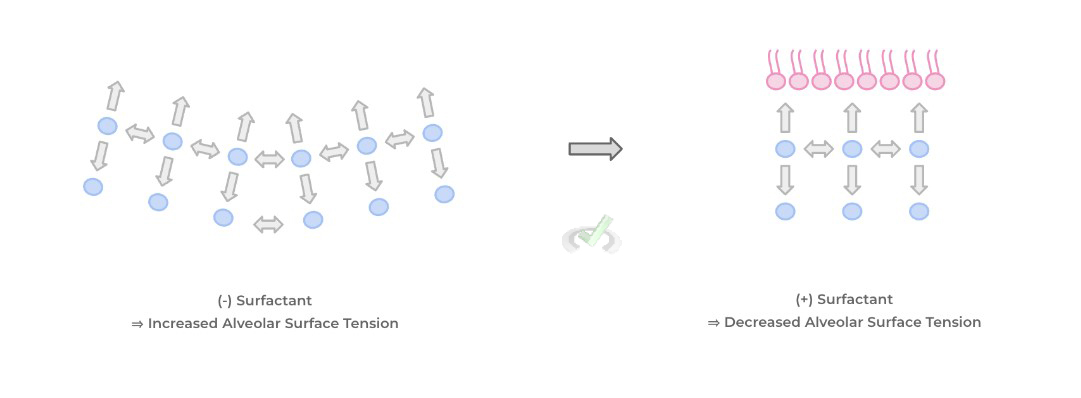
Type 2 pneumocytes secrete a substance called surfactant, which is an important amphoteric molecule which is important in reducing alveolar surface tension from the alveolar fluid in order to prevent their collapse and keep the alveoli open!
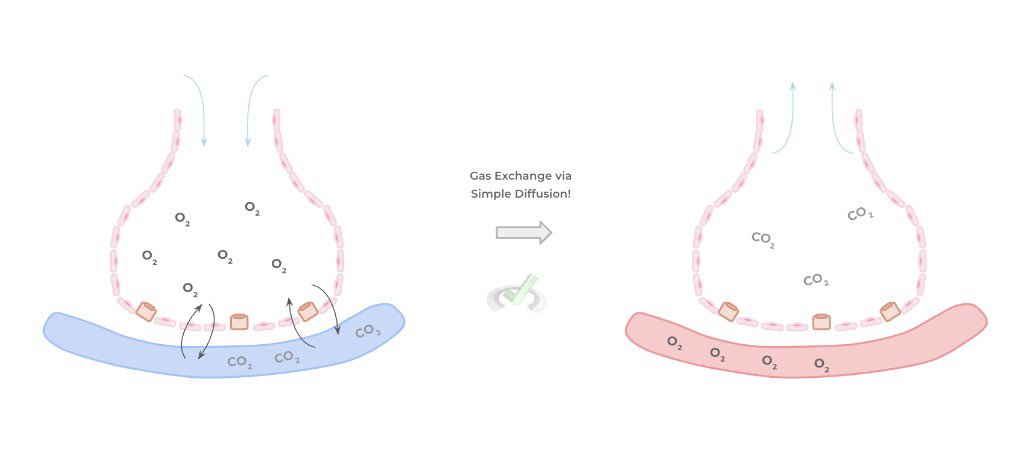
The process of gas exchange in the alveoli is actually fairly simple, occurring via simple diffusion! Because the inhaled air has a higher O2 concentration than the incoming blood in the alveolar capillaries, O2 diffuses down its concentration gradient to reoxygenate the blood.
Conversely, the high CO2 concentration in the blood diffuses down its gradient into the low CO2 concentrated alveolar air which is then exhaled!
III. Bridge/Overlap
When we use the word amphoteric to describe the surfactant molecule, you may have a bell ring off in your head saying that you’ve seen this word before! You’re exactly right because it’s the same word used to describe phospholipids of the cell membrane! Let’s see why this amphoteric nature is so crucial to the function of surfactant!
I. Amphoterism and Role in Reducing Surface Tension
Recall that an amphoteric molecule refers to a molecule which has a hydrophilic (“water loving”) and a hydrophobic (“water fearing”) component. In this case, surfactant possesses this amphoteric character due to the various phospholipids it contains, particularly dipalmitoyl phosphate!
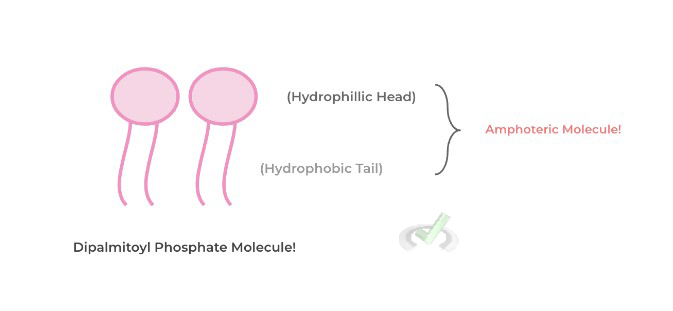
Surface tension refers to the attraction of a liquid’s molecules towards one another on the surface which results in a subsequent reduction in surface area. As such, we can see why increased surface tension of the alveolar fluid could cause a detrimental collapse of the alveoli.
Surfactant combats this by reducing this attraction of molecules whereby the hydrophilic component interacts with the alveolar fluid molecules and prevents them from having interactions with one another thereby reducing surface tension and preventing alveolar collapse.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Upper and Lower Respiratory System
The respiratory system can be divided into an upper and lower tract with the main divider between the 2 being the epiglottis!
I. Upper Respiratory Tract
The 4 main structures of the URT include the nose, nasal cavity, the mouth, and the pharynx. Air can be inhaled from the nose into the nasal cavity or via the mouth and make their way into the pharynx, a muscular tube-like structure behind both the nose and the mouth.
Because the pharynx leads both into the esophagus and the larynx, the epiglottis is a specialized structure of hyaline cartilage which can close the larynx during food consumption so that food only enters the esophagus into the alimentary canal!
II. Lower Respiratory Tract
The lower respiratory tract includes the larynx, trachea, as well as the major subdivisions of the respiratory tract! The larynx contains your vocal cords which aid in producing sound and leads into your trachea (a.k.a windpipe) which marks the beginning of your lungs.
The trachea breaks off into primary bronchi: one for the right lung and one for the left. The bronchi then divide into smaller bronchioles which then eventually lead into the alveoli, sac-like structures where gas exchange occurs!III. Lung Lobes and the Pleural Cavity
The lungs can be divided into various lobes: 3 lobes for the right lung (superior, middle, and inferior) and 2 lobes for the left lung (superior and inferior), all of which are separated by fissures.
The lungs are also encased in the pleural cavity, which is a 2 membraned sac containing the visceral and parietal pleura. Like the pericardial sac, the pleural cavity has function in protection and lubrication while breathing!
B. Alveolar Structure and Gas Exchange
The alveoli are sac shaped structures which are lined by a simple squamous epithelium of alveolar cells. There are 2 types of alveolar cells: type 1 and 2 pneumocytes.
Type 1 pneumocytes are most abundant and are the main participants in gas exchange while type 2 pneumocytes secrete surfactant in order to reduce surface tension!
Gas exchange occurs via simple diffusion as the incoming inhaled air is high in O2 and moves down its concentration to oxygenate the blood. Conversely, the high CO2 concentration in the blood diffuses into the CO2 poor alveolar air which can then be exhaled!
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
Which of the following structures is the last common point where the GI/alimentary tract and respiratory tract meet?
A. Nasal Cavity
B. Mouth
C. Trachea
D. Pharynx
Answer: D. Pharynx
The pharynx is the last common point of the GI/alimentary and respiratory tract meet as the pharynx, a muscular tube like structure behind the nose and mouth, can lead into either of these tracts. The trachea is the beginning of the lungs and comes after the larynx which is also a part of the lower respiratory tract.
Sample Practice Question 2
Infant respiratory distress syndrome is a breathing disorder for infants which stems from the immature development of type 2 pneumocytes. Which of the following physiological consequences will result from this?
I. Decreased Surfactant Production
II. Increased Alveolar Surface Area
III. Decreased Surface Tension
A. I only
B. II only
C. III only
D. I and III
Answer: A. I only
Because there is deficient production of type 2 pneumocytes, there will also be a deficient production of surfactant. As a result, there would be increased alveolar surface tension resulting in alveolar collapse which would lead to a decrease in alveolar surface area for gas exchange.



 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these 

 reviews on TrustPilot
reviews on TrustPilot