I. What are the Functions of the Excretory System?
The idea of balance is something we can apply to our everyday lives and can give us a little peace of mind and serenity. Whether we’re talking about a work-life balance, a balance of our finances, or a social balance with our relationships, this is definitely something that we could incorporate into our daily routine.
In a similar way, our kidneys function to maintain homeostasis within our body in various ways! In this article, we’ll go ahead and touch on how the kidneys maintain this physiological balance on a grand scale while in other articles, we’ll touch on the specific details on how it accomplishes this!
II. Homeostatic Function of the Excretory System
Though the name of the system implies excretion must occur — which is definitely true — the kidneys, which are the main organs of the excretory system, are better thought of as a “filter” as there’s a need to excrete toxic substances but also filter and retain the wanted molecules such as to maintain homeostasis.
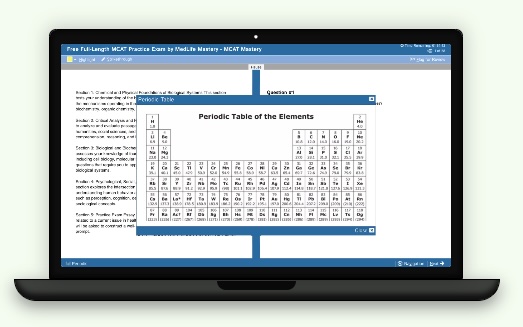
A. Blood Filtration and Urine Formation
As mentioned, it’s better to think of the kidneys as a filter as they filter incoming blood in order to retain needed molecules and excrete toxic ones.
The excreted molecules combined with excess fluid eventually form urine which is then excreted via the urinary system — these 2 processes occur at the functional unit of the kidneys called nephrons which we go into much more detail in another article!
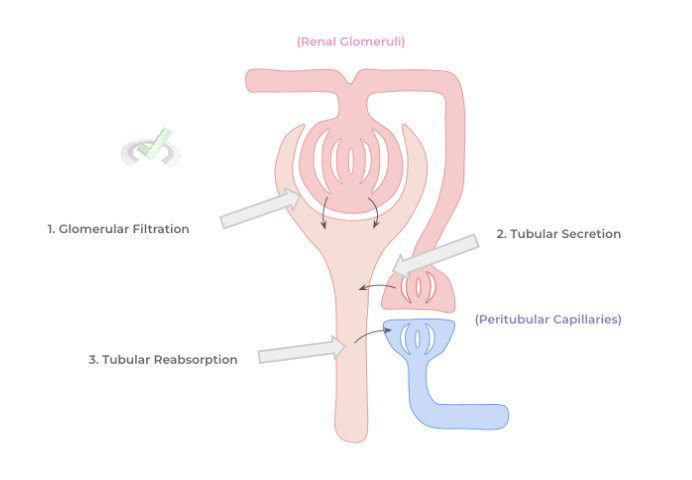
As seen from above, there are 3 main processes that occur in order to allow both blood filtration and urine formation: glomerular filtration, tubular secretion, and tubular reabsorption — these terms will be better understood when we touch on nephron structure in a subsequent article.
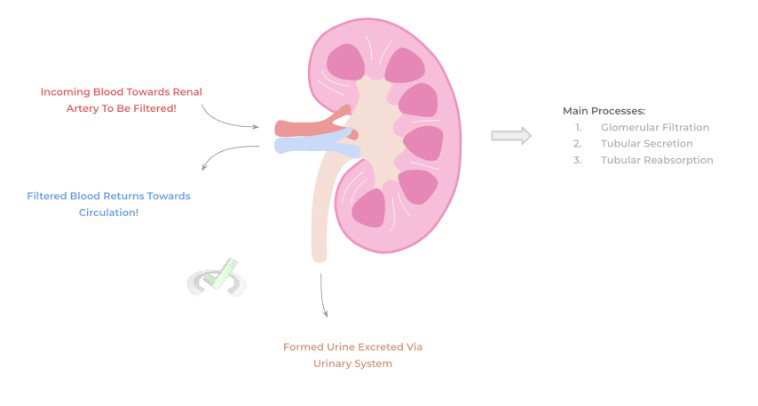
To give a quick overview, glomerular filtration is the first step where incoming blood from the renal artery enters into a special type of capillary structure called the renal glomeruli.
These capillaries are unique as they are fenestrated (“having holes”) which allows for incoming blood to be initially filtered so that no critical proteins or cells enters the filtrate, which is the fluid that passes through the glomeruli and further continues down the nephron to eventually form urine.
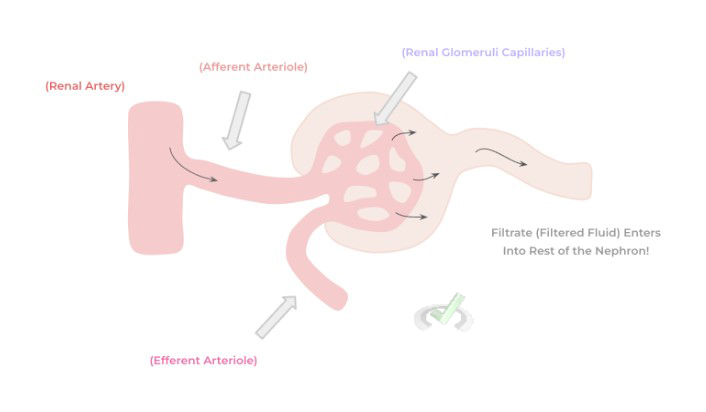
The filtrate then enters into the remaining nephron tubule where secretion and reabsorption can occur: secretion refers to molecules from the blood ENTERING INTO the tubular filtrate while reabsorption indicates molecules from the filtrate ENTERING BACK into the blood.
Note that the efferent arteriole shown above actually continues its path after the glomeruli traveling adjacent to the tubular nephron forming peritubular capillaries — these are the blood vessels that interact with the nephron to allow for the reabsorption and secretion of molecules.
It’s through tubular secretion and reabsorption that the kidney’s can maintain a homeostatic balance of blood electrolytes which is crucial on a cellular level, particularly for maintaining membrane potential, as well as blood acid-base balance via the secretion/reabsorption of bicarbonate!
B. Maintenance of Blood Pressure and Blood Volume
In addition, reabsorption capacity of blood is not just limited to important blood electrolytes, but also involves the reabsorption of water back into the bloodstream to maintain blood volume and pressure — this section might be a little review of some of the actions of the endocrine hormones, particularly aldosterone and vasopressin/antidiuretic hormone.
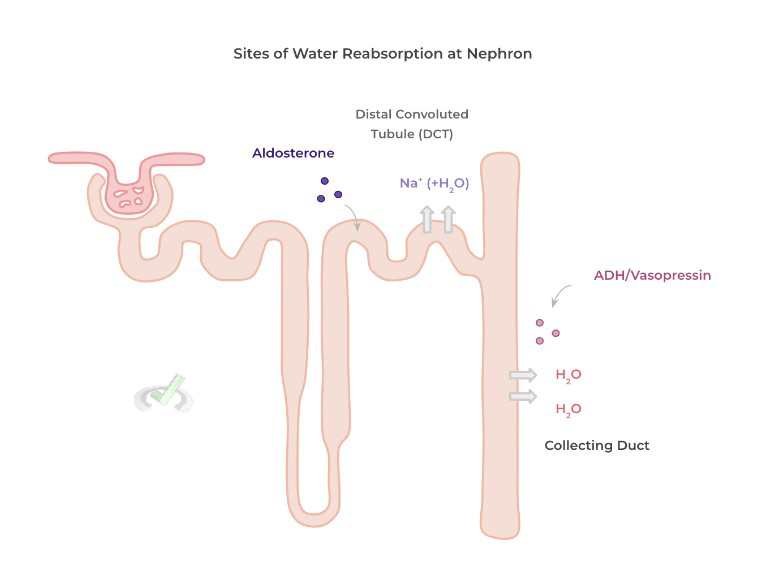
Water reabsorption in the nephron occurs at 2 sites: the distal convoluted tubule and the collecting duct which are stimulated by the hormones aldosterone and vasopressin/antidiuretic hormone, respectively.
Upon the sensing of decreased blood pressure via baroreceptors within the renal tubular epithelial cells, these hormones are released and act on the nephron to induce water reabsorption which would result in an increase in blood volume and thus blood pressure.
C. Release of Endocrine Hormones
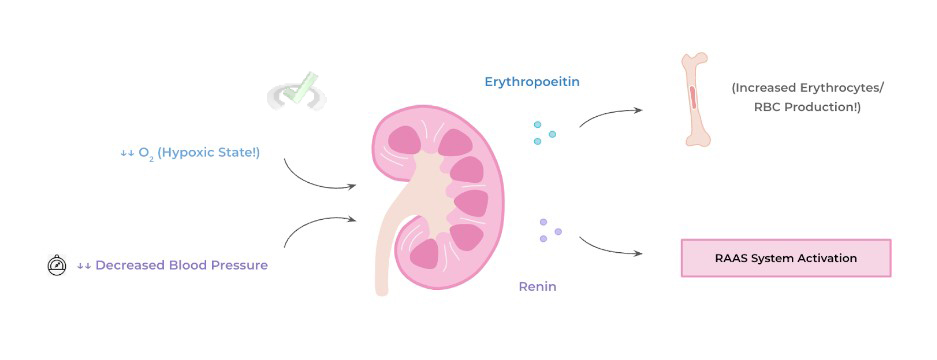
Finally, while it doesn’t seem so on the surface, the kidney is actually also an endocrine organ as it releases 2 main hormones: erythropoietin and renin. Erythropoietin is released under conditions of hypoxia because of its ability to increase red blood cell production, called erythropoiesis!
The released renin is the same renin associated with the renin-angiotensin-aldosterone system! Having dual function as a hormone and enzyme, renin is released under decreased blood pressure in order to activate the RAAS system to increase water reabsorption and increase blood volume!
III. Bridge/Overlap
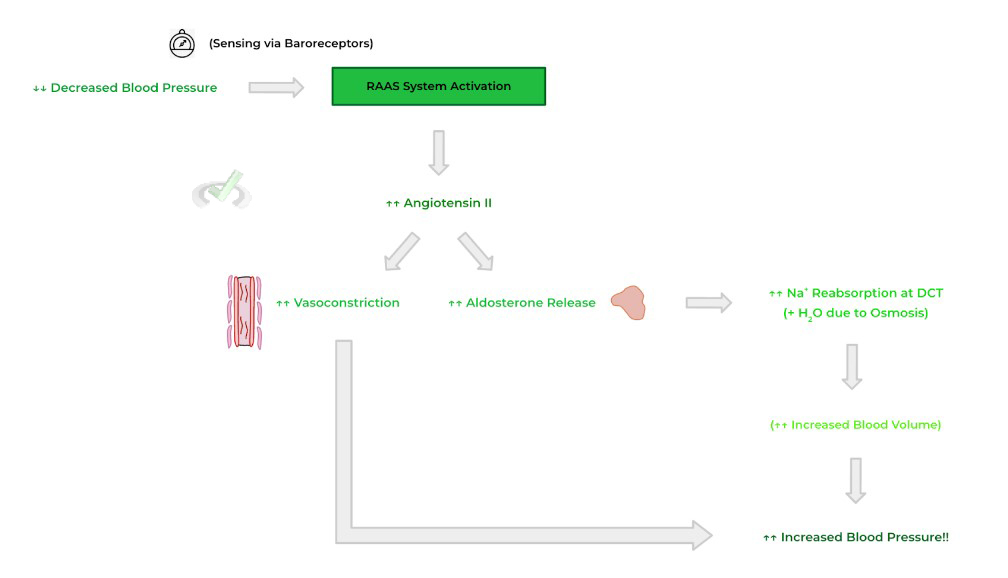
As we touched on the nephron’s role in water reabsorption and maintaining blood pressure and volume, it may be helpful to get a quick review on one of the pathways! Let’s go ahead and review how the RAAS system is activated as its pathway is a bit longer than most endocrine pathways.
I. Review of the Renin-Angiotensin-Aldosterone System
The RAAS system is activated in response to low blood pressure, detected via baroreceptors located in the renal tubular epithelial cells! This allows for the release of renin by the kidney, which is a proteolytic enzyme which initiates cleavage of angiotensinogen (which is released by the liver) to angiotensin I.
Angiotensin I is then converted into angiotensin II via the angiotensin converting enzyme (ACE) located in the lungs! Angiotensin II can increase blood pressure in a variety of ways including vasoconstriction and allowing for the release of aldosterone by the adrenal gland.
Finally, the released aldosterone can bind to receptors located in the distal convoluted tubule of the nephron to allow for sodium reabsorption and consequently water reabsorption due to osmosis which increases blood volume and thus increases blood pressure.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Blood Filtration and Urine Formation
The filtration of blood allows for important needed molecules to be retained while excreting unwanted, toxic metabolites. The excreted molecules in addition to the excess fluid filtered from the blood results in the filtrate which eventually becomes urine to be excreted via the urinary system.
There are 3 main processes involved in blood filtration and urine formation: glomerular filtration, tubular secretion, and tubular reabsorption. Glomerular filtration involves the initial filtering of blood at the renal glomerulus which filters out proteins and cells from the filtrate.
Tubular secretion refers to the movement of molecules from the bloodstream into the filtrate while tubular reabsorption refers to movement of molecules from the filtrate back into the bloodstream!
B. Maintenance of Blood Pressure and Blood Volume
Water can also be reabsorbed from the filtrate back into the bloodstream in order to increase blood volume and thus increase blood pressure! The 2 main hormones which can enact water reabsorption in the nephron are aldosterone and vasopressin/antidiuretic hormone.
When low blood pressure is detected via the baroreceptors, aldosterone and vasopressin are released and act on the distal convoluted tubule and collecting duct, respectively, to allow for water reabsorption back into the bloodstream!
C. Release of Endocrine Hormones
The kidneys also have endocrine function as they allow for the release of erythropoietin and renin. Erythropoietin is released due to hypoxia in order to generate more erythrocytes while renin is released when blood pressure is decreased in order to activate the RAAS system!
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
When examining the urine, a nephrologist notices that the urine has a red color possibly indicating the presence of blood. As such, which of the following nephron structures is dysfunctional and is leading to this problem?
A. Glomerular Filtration
B. Tubular Secretion
C. Tubular Reabsorption
Ans. C. Tubular Reabsorption
Recall that the activation of the RAAS system ultimately results in increased blood pressure via the reabsorption of sodium and consequent reabsorption of water via osmosis! As such, tubular reabsorption is heightened via the activation of the RAAS system.
Sample Practice Question 2
In cases of increased blood loss due to hemorrhage, which of the following would you expect to be increased?
I. Erythropoietin Release
II. Aldosterone Release
III. Vasopressin Release
A. I and II
B. I and III
C. II and III
D. I, II, and III
Ans. D. I, II, and III
This is a really great example of how MCAT questions will require you to think and analyze problems in the context of scenarios! Blood loss due to hemorrhage would result in both hypoxia (due to a loss of RBCs) and blood pressure (due to a loss of blood volume).
As such, all of the above would be increased as erythropoietin would induce erythropoiesis to counteract the loss of RBCs will aldosterone and vasopressin would work at the nephron to stimulate water reabsorption and increase blood volume (and thus blood pressure).



 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these