I. What is Immunological Antigen Presentation?
It’s funny how the phrase “presentation is everything” can apply to so many things within our lives. You can hear the top Michelin star chefs hound this phrase when it comes to the plating of food or even how your parents tell you to dress well for a formal event in order to look presentable.
The immune system is exactly the same way when it comes to the presentation of antigens, self or pathogenic, to various immune cells in order for a proper monitoring of the various cells of the body to see if the body is in a healthy state or if there’s a possible infection of inflammatory disease that’s occurring. Let’s go ahead and get into how the immune cells allow for such monitoring to occur!
II. Presentation of Self and Pathogenic Antigen Presentation
Let’s go ahead and define first what an antigen is: an antigen is a molecule, often a protein, that can be recognized by one’s immune system. Note that there are 2 types of antigens: self-antigens and pathogenic antigens.
Self antigens are simply the molecules that originate from the host tissue and SHOULD NOT stimulate immune cells to stimulate an inflammatory response — when this system goes wrong, an autoimmune reaction occurs! Pathogenic antigens are foreign antigens, most often proteins coming from infectious microorganisms which should activate immune cells to trigger an inflammatory response!
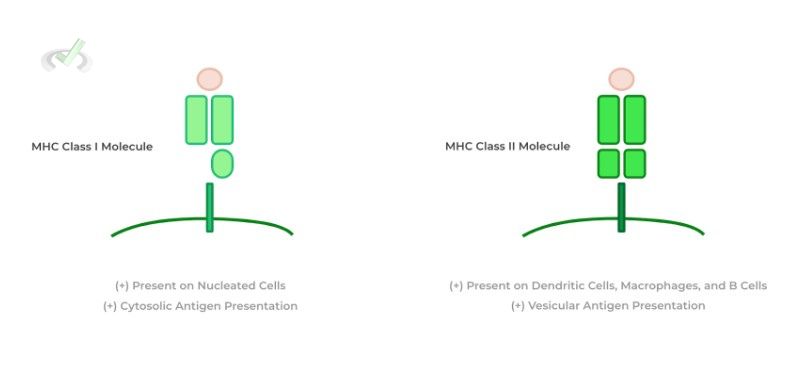
A. MHC Class Molecules
The various cells of the body can present these antigens to the cells of the immune system via specialized presentation proteins called MHC class molecules. These proteins take other proteins (either self or pathogenic antigens) and present them on the cell surface to immune cells to inform the immune system if an infection or diseased state has taken place!
There are 2 main types of MHC class molecules which have specific characteristics and are presented on different cells: 1) MHC class I and 2) MHC class II. MHC class I molecules are expressed on ALL NUCLEATED cells and allow for presentation of cytosolic antigens.
In contrast, MHC class II molecules are only expressed on 3 specific immune cells: dendritic cells, macrophages, and B cells and present antigens which originate from the vesicular pathways.
B. Exogenous v.s. Endogenous Pathways for Antigen Presentation
The next big difference in regards to the antigen presentation is whether the antigen originates from the cytosol or the vesicular pathway as we described above.
In short, antigens which are derived from the cytosol will be presented via the endogenous pathway utilizing MHC-I class molecules. Conversely, antigens which are derived from the vesicular pathway will be presented via the exogenous pathway utilizing MHC-II class molecules.
I. Endogenous Pathway
The best word to associate with this pathway is intracellular in the sense that the antigens originate from the intracellular cytosol. Additionally, associate this pathway with the presentation of viral antigens because these are obligately intracellular pathogens that utilize the cytosol for replication!
Once these viral proteins are released into the cytosol during replication, these proteins can be taken up and proteolytically cleaved in a process called antigen processing so that the antigen can fit nicely in the antigen site of the MHC-I molecule.
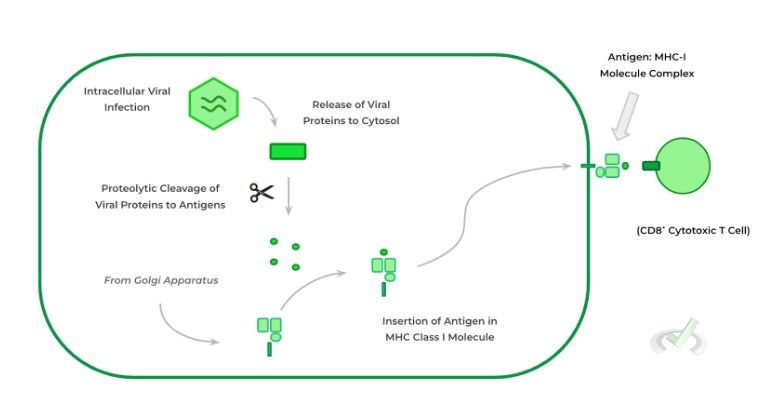
Additionally, another important thing to note is that this presentation of antigens isn’t just limited to anytime there’s a viral, intracellular viral infection, but even occurs when no infection is present in which case the presented antigens are self-antigens!
In this case, the T cells (ideally) don’t reactive to the presented self-antigens as they have undergone negative selection and simply “gloss” over the healthy cell. This pathway is even active when cancer is present where the presentation of cancerous antigens is presented via the endogenous pathway.
II. Exogenous Pathway
In contrast, the best word to associate with the exogenous pathway is either phagocytosis or endocytosis as the antigens must be uptaken via either these mechanisms — this is why antigens in this pathway originate in the vesicular system due to these processes!
Usually either a pathogenic protein or more commonly the actual microorganism which is uptaken via phagocytosis/endocytosis and are uptaken into vesicles called endosomes.
These endosomes then fuse with lysosomes which contain enzymes which also proteolytically process the exogenous proteins into antigens. Finally, the processed antigens are then incorporated into MHC-II molecules and expressed on the cell surface to present.
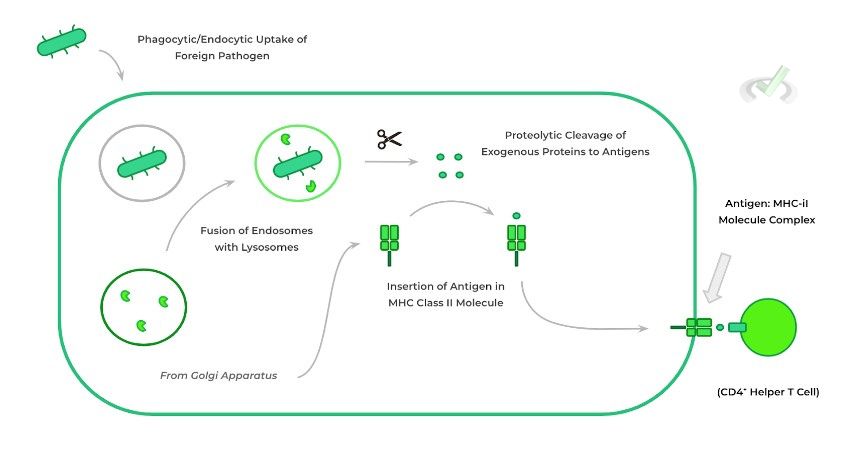
Being that the endogenous pathway utilizes MHC-II molecules, it follows that only dendritic cells, macrophages, and B cells can partake in this pathway as these are the only cells which have MHC-II molecules!
Conversely, all nucleated cells can participate in the exogenous pathway because all nucleated cells express the MHC-I molecules! Take a look at the table below to get a quick summary of the differences between the endogenous and exogenous pathways of antigen presentation!

III. Bridge/Overlap
You may have noticed that based on the pathway, certain T cells will be activated — CD8+ cytotoxic T cells for the endogenous pathway and CD4+ helper T cells for the exogenous pathways. Let’s go ahead and review some of the main differences between these 2 different T cells.
I. Differences in Function and Action of Cytotoxic and Helper T Cells
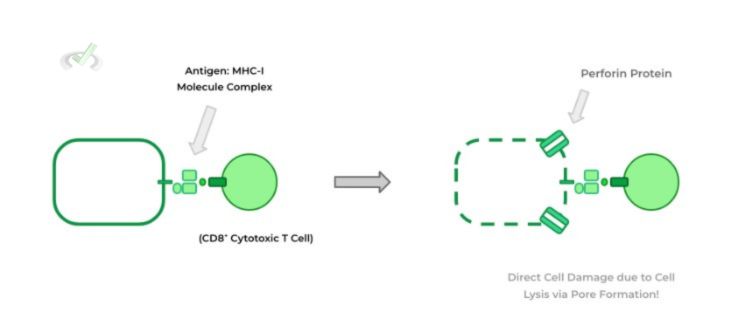
The main difference in regards to the action of the cytotoxic and helper T cells is whether they cause direct or indirect cell death for infected cells. In the case for cytotoxic T cells, the activation of these CD8+ cells causes DIRECT cell damage.
This occurs through a variety of mechanisms, particularly via pore formation via perforin — this induces cell lysis which results in cell damage of the affected cell. This explains why all nucleated cells express MHC-I as all these cells are susceptible to viral, intracellular infection — the activation of CD8+ cytotoxic T cells via the endogenous pathway can allow for direct killing of the infected cells.
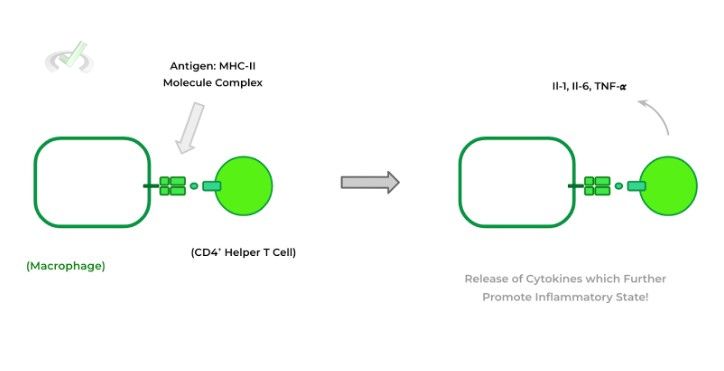
Conversely, the activation of T helper cells primarily via macrophages through the exogenous pathway of antigen presentation triggers the T helper cells to release various amounts of immunostimulatory proteins called cytokines which allows for the promotion of the inflammatory response — these physiological changes can include increase vascular permeability, immune cell recruitment, etc.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. MHC Class Molecules
Cells across the body allow for the presentation of antigens via MHC class molecules in order to alert the body if there is an infectious or inflammatory state present. There are 2 types of MHC class molecules each with distinct characteristics: MHC class I and MHC class II molecules.
MHC class I molecules are present on ALL NUCLEATED cells and present antigens which are derived from the cytosol. MHC class II molecules are present on certain cells, particularly dendritic cells, macrophages, and B cells and present antigen derived from the vesicle system.
B. Exogenous v.s. Endogenous Pathway for Antigen Presentation
There are 2 different pathways of antigen presentation where the determining factor for which presentation is used is the origin of the antigen: the exogenous and endogenous pathways!
I. Endogenous Pathway
The best word to associate the endogenous pathway with is intracellular as antigens come from the intracellular cytosol. Most commonly, the antigens presented in this pathway are viral because they are an intracellular pathogen!
After the release of pathogenic proteins in the cytosol during viral replication, the proteins undergo proteolytic cleavage in a process called antigen processing. The antigens are then placed on MHC class I molecules and are then expressed on the surface of the cells to be presented on CD8+ cytotoxic T cells.
II. Exogenous Pathway
Conversely, the best word to associate with the exogenous pathway is phagocytosis or endocytosis as the antigens which are presented on the exogenous pathway are derived from endosome vesicles which uptake the antigens extracellularly!
After uptake, the endosome vesicles with the antigens fuse with lysosomes which also contain proteolytic enzymes to allow for antigen processing. The antigens are similarly placed on the MHC class II molecules and are then expressed on the surface of the specialized cells to be presented on CD4+ helper T cells!
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
Suppose there’s a genetic condition where a misfolding occurs in the MHC class I molecule and results in their faulty expression on cell surfaces. Which of the following cells would be most likely affected as a result of this condition?
I. Erythrocytes (Red Blood Cells)
II. B Cells
III. Endothelial Cells (Epithelial Lining of Blood Vessels)
A. I only
B. III only
C. I and III
D. II and III
Ans. D
This question requires a little bit of prior knowledge as well as being very attentive to the characteristics of MHC class I molecules. Recall that MHC class I molecules are antigen presenting proteins present on the surface of all NUCLEATED cells. Being that erythrocytes are not nucleated, they would not be affected by this condition. However, B cells and endothelial cells are nucleated which will result in them being affected by a lack of MHC class I molecule expression.
Sample Practice Question 2
Legionella pneumophila is a type of obligate intracellular parasite which can infect respiratory epithelial cells. As such, which pathway and which MHC class molecule would most likely be used to present this antigen towards the respective immune cells?
A. Endogenous, MHC-II
B. Exogenous, MHC-II
C. Endogenous, MHC-I
D. Exogenous, MHC-II
Ans. C
In this case, because the microorganism is an intracellular organism, the antigens will most likely be derived from the cytosol due to the intracellular course of infection. These will then be presented via the endogenous pathway and placed in MHC-I molecules



 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these