I. What are the Cells of the Innate and Adaptive Immune System?
The phrase “it really does take a village/army” can be perfectly adapted to the wide variety of cells of the immune cells. It’s truly amazing to see all these cells which have individual specific functions all come together in order to serve an overlying main purpose: to protect the body from foreign invaders trying to establish infection!
It can for sure be a little daunting and scary when you first look at all the different cells of the immune system with all their different functions and characteristics. However, as with all things here in Medlife Mastery, breaking things down and categorizing them makes things much easier to learn and comprehend. Let’s go ahead and dive into the various cells which work to protect us from infection!
II. Innate Immune Cells v.s. Adaptive Immune Cells
As their name implies, innate immune cells are the cellular components which are associated with innate immunity while adaptive immune cells are specialized for generating the adaptive immune response!
Recall that the innate immune system is your subdivision of your immune system which is “always activated” as there are an abundant amount of innate immune cells circulating throughout the body ready to immediately fight infection whenever present!
Conversely, the adaptive immune response is your immune response which is known for its specificity in regards to pathogen killing due to the presence of specific receptors. However, this immune response is much slower and occurs longer in duration in order for clonal selection to choose specific T/B cells and cause them to proliferate! Take a look at the summarized diagram below of all the cells we’ll be covering!
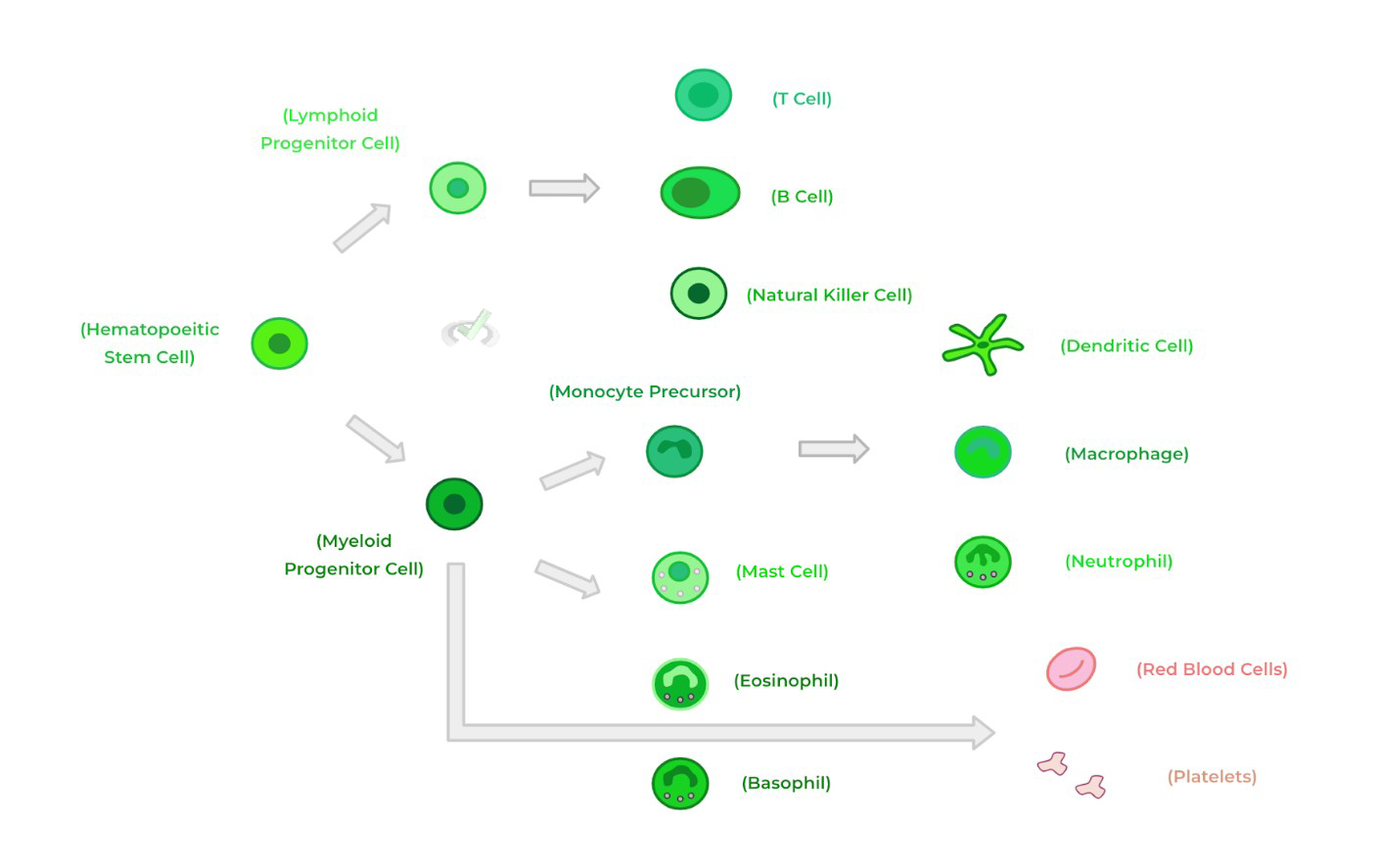
A. Innate Immune Cells
Though the number and wide range of innate immune cells can seem a little bit daunting at first, it definitely helps to have some sort of categorization in order to make the division of innate immune cells much easier!
There are 2 main categories we can divide the various immune cells into: 1) granulocytes and 2) agranulocytes. The two categories of cells basically differ in regards to the presence of cytoplasmic granules which contain various proteins and molecules which aid in the immune response!
I. Granulocytes
There are 4 main types of granulocytes: neutrophils, eosinophils, basophils, and mast cells — all of them have the main commonality of having cytoplasmic granules containing various immune promoting molecules!
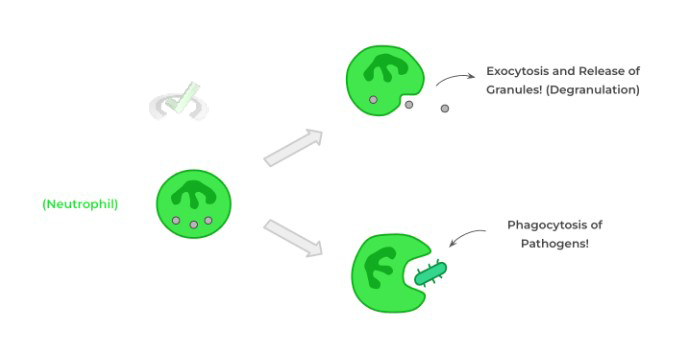
Neutrophils are actually the most abundant immune cell within the body as they constantly circulate throughout the blood ready to enter tissues should there be infection. In addition to releasing their granules which contain various immune molecules which suppress infection, neutrophils also allow for phagocytosis of pathogens!
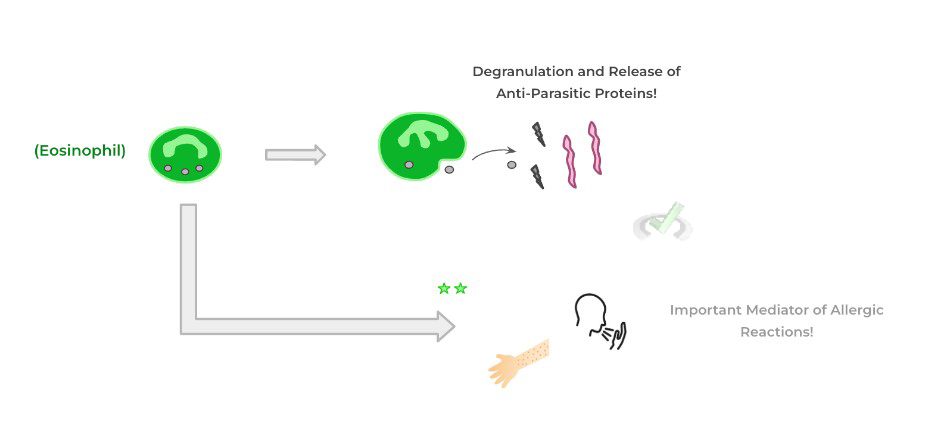
Eosinophils are another type of granulocyte which has a more specialized function in the sense that the molecules released during degranulation are particularly toxic to parasitic infections! However, they’re also involved in the mediation of allergic and hypersensitivity reactions.
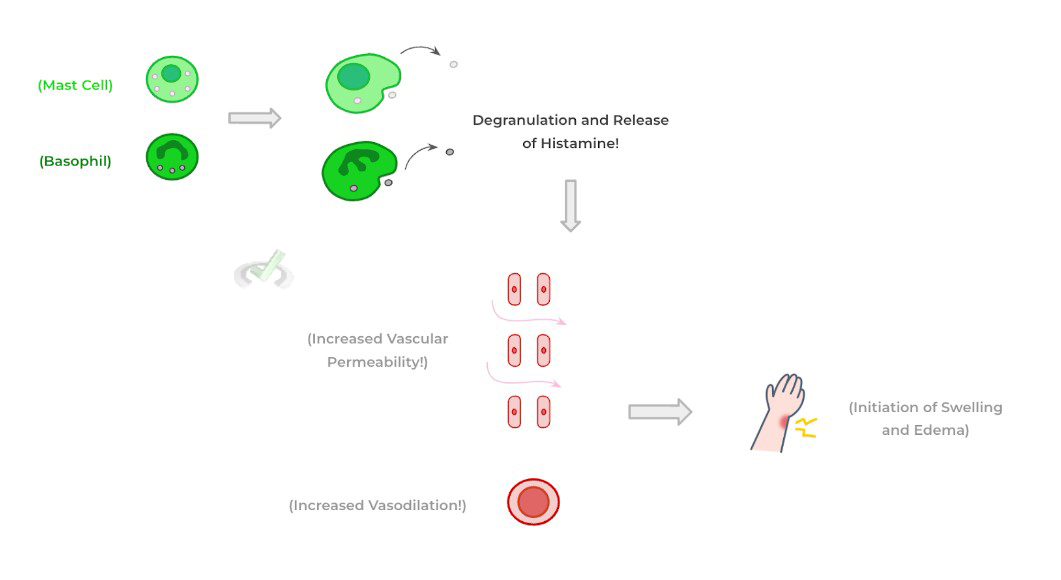
Finally, we’ll clump basophils and mast cells together as they are both similar in the sense that their granules contain histamine, which is an important immunostimulatory molecule! However the physiological effects of histamine are generally more prominent when released by mast cells as basophils make up the smallest percentage of circulating immune cells.
The main physiological effects of histamine are to increase vasodilation and increase vascular permeability: these combined effects allow for increased blood plasma to enter into the tissue with the immune cells and mediators to promote inflammation should infection be present!
II. Agranulocytes
As their name implies, agranulocytes are innate immune cells which DO NOT contain granules within their cytoplasm: these innate immune cells primarily include natural killer cells, macrophages, and dendritic cells.
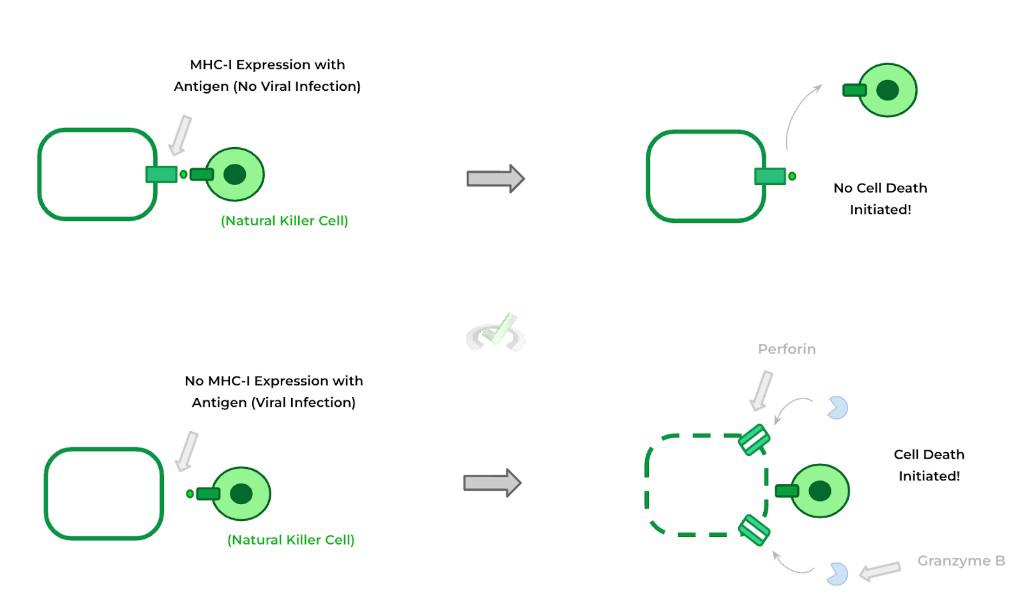
As you’ll see soon, natural killer cells are essentially the innate immune cell equivalent of cytotoxic T cells as they are mediated in the DIRECT CELLULAR killing of viral infected cells. They do this by looking for cells with a down regulation of MHC class molecules which indicates viral infection.
NK cells then kill these virally infected cells by embedding a pore forming protein called perforin — once the pore is formed, the NK cells inject proteolytic enzymes called granzymes which initiates a cell death cascade! As we’ll cover later, this is the exact same mechanism by which cytotoxic CD8+ T cells kill infected cells!
Macrophages are another important type of phagocyte similar to neutrophils and dendritic cells (as we’ll touch on). In opposition to neutrophils, macrophages are termed “resident phagocytes” as they don’t circulate but instead primarily reside in various tissues around the body!
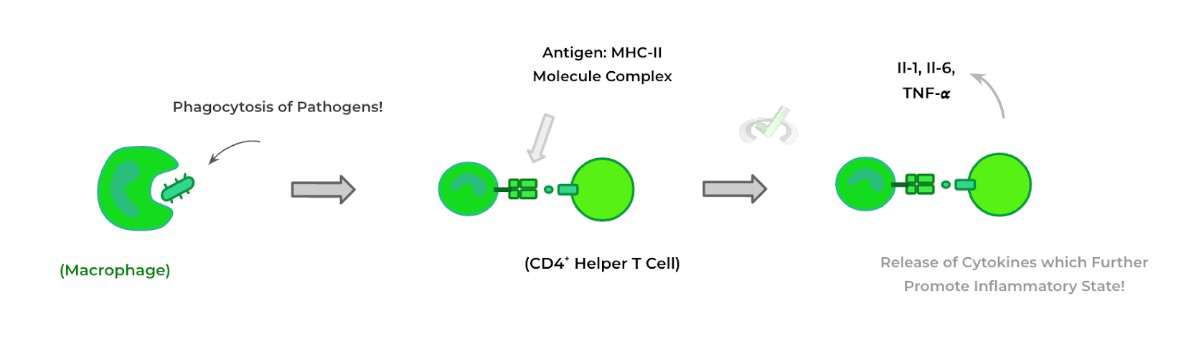
Within the tissues, macrophages can phagocytose pathogens and then present them on MHC-II molecules in order to activate CD4+ T helper cells — these activated T helper cells can then secrete various cytokines, which are immunostimulatory molecules to further promote the inflammatory response!
Finally, we left dendritic cells for last because of their importance as acting as the “bridger cell” between the innate and adaptive immune system. Similar to neutrophils and macrophages, dendritic cells are phagocytes and also circulate and remain within tissue — though, their biggest effects are as resident tissue phagocytes.
Should an infection be present, dendritic cells can phagocytose pathogens within the tissue. From here, they then travel via the lymphatic vessels towards lymph nodes and present the processed antigen to the present T and B cell lymphocytes with the hope that some of the lymphocytes bear the receptors specific for the pathogenic antigen!
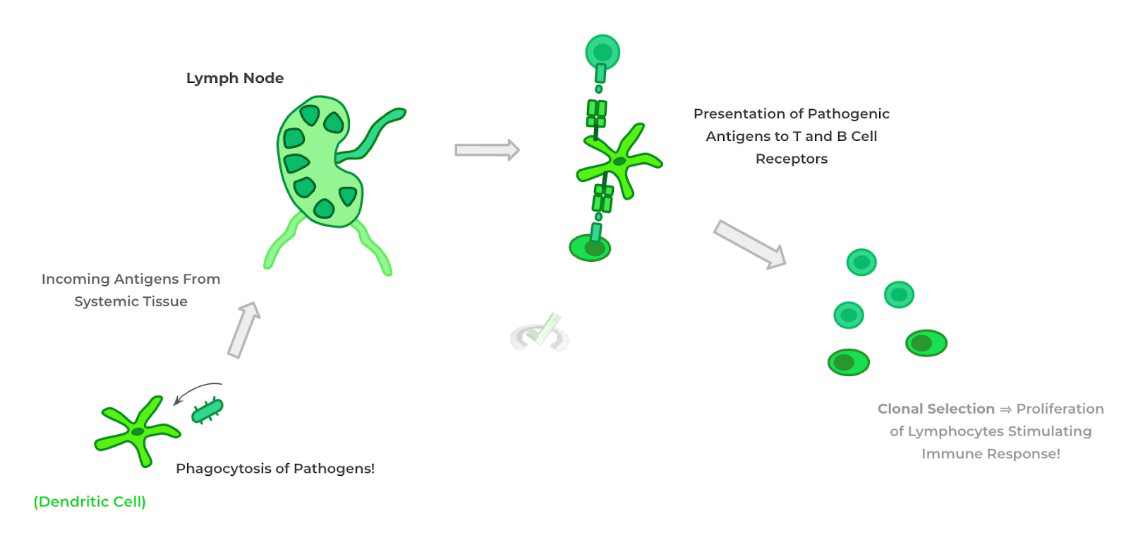
It’s because of this that you can appreciate how dendritic cells are referred to as the bridge between the innate and adaptive immune system! With this, let’s transition into the cells of the adaptive immune system!
B. Adaptive Immune Cells
Let’s now get into the cells of the adaptive immune system - recall that the adaptive immune response is your more specialized immune response as it selects for lymphocytes with specific receptors for a particular pathogenic antigen. Luckily, there are only 2 adaptive immune cells to know abouts: T and B cell lymphocytes.
I. T Cell Lymphocytes
These lymphocytes get there name because these immune cells complete maturation in the thymus after initial maturation in the bone marrow.
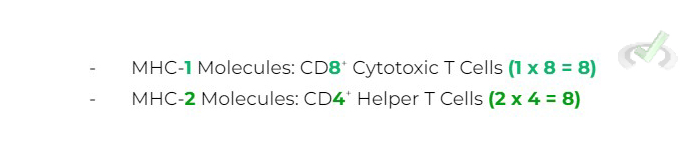
There are 2 types of T lymphocytes which are involved in cell-mediated immunity: CD8+ cytotoxic and CD4+ helper T cells — the CD4/8 nomenclature refers to the co-receptor proteins found on the respective T cells which also bind to the MHC class molecule!
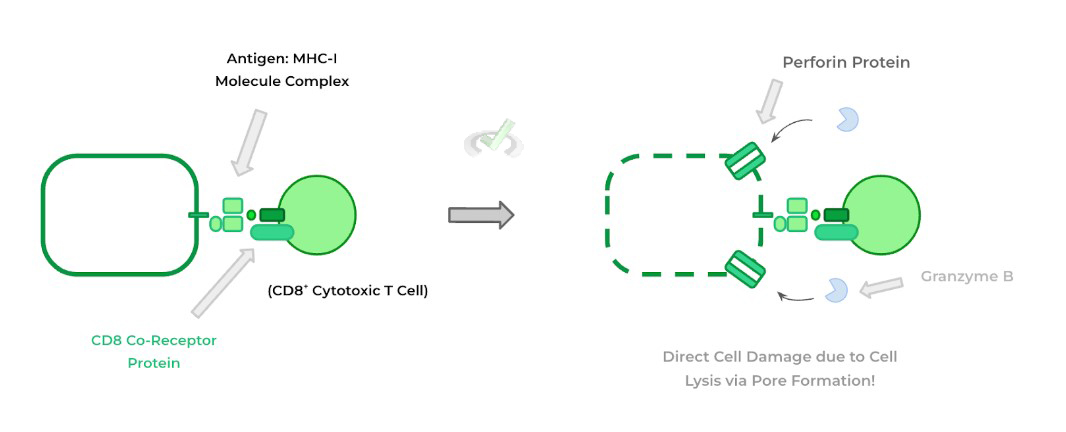
CD8+ cytotoxic T cells are involved in the DIRECT CELL killing of infected/cancerous cells in a very similar way to NK cells. The main thing to understand about the CD8+ T cells is that they recognize antigens presented on MHC-I molecules.
Once the specific T cell receptors recognize their pathogenic antigens present on the MHC-I molecules, they have a similar mechanism of perforin insertion and granzyme B release which mediates cell death!
CD4+ T helper cells are more responsible for INDIRECT cell mediated death in the sense that they don’t directly kill the cell, but allow for the release of the appropriate pro-inflammatory cytokines which will eventually lead to cell killing! Recall again that T helper cells are activated by macrophages through the presentation of antigens via MHC-II molecules!
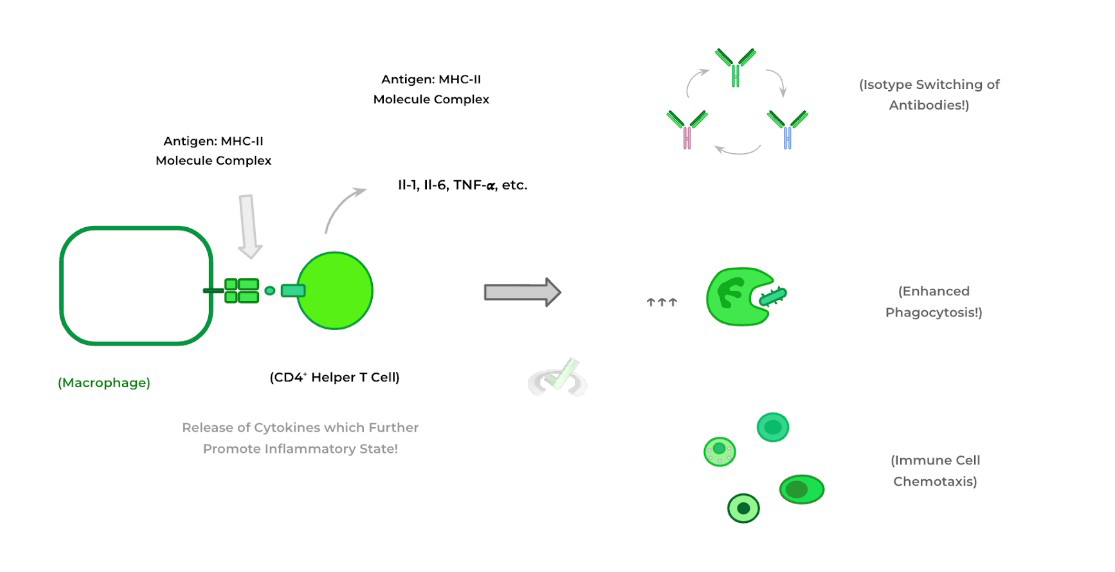
The release of these pro-inflammatory cytokines can result in various downstream effects which contribute to the inflammatory response such as increasing macrophage phagocytosis, isotype switching of antibodies, immune cell recruitment (chemotaxis), etc. as shown above!
Again, it’s important to understand that there’s a specificity where the CD8+ cytotoxic T cells recognize MHC-1 molecules and CD4+ helper T cells recognize MHC-II molecules. To help remember this, try and use the “8 Multiplication” Rule as shown below!
II. B Cell Lymphocytes
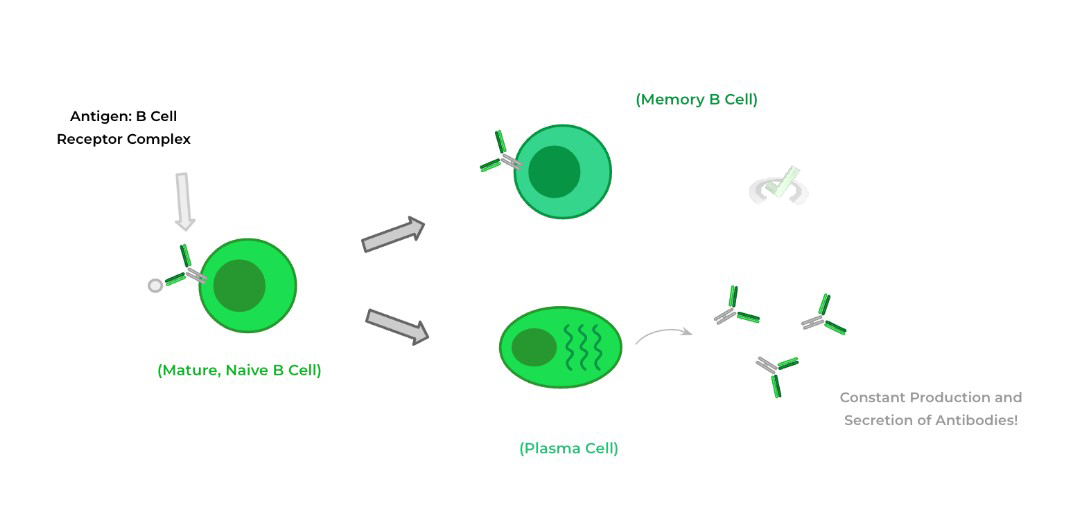
Similarly, these lymphocytes get their names from completing their entire maturation in the bone marrow. The main function of B cells is the production of antibodies which are soluble, Y shaped proteins within the blood that aid in the eradication of pathogens through a variety of mechanisms as we discuss in further detail in another article.
To be more specific, once a B cell and its receptor (which is actually an antibody protein but still bound to the membrane) recognizes its antigen, it then differentiates into a plasma cell and a memory B cell.
The plasma cell is a differentiated version of the B cell which constantly produces and secretes antibodies into the bloodstream while the memory B cells acts as a reservoir to stimulate a faster secondary immune response should the infection occur again.
III. Bridge/Overlap
If you’ve covered other articles talking about cells of other organ systems, you may have already encountered various macrophages without even knowing about them! Let’s go ahead and look at some examples of macrophages in various tissues scattered throughout the body!
I. The Resident Macrophages of the Human Body
Recall that macrophages are best described as resident tissue macrophages which allow for phagocytosis of pathogens and presentation of their antigens to T helper cells. Being that they reside in various tissues throughout the body, have a look below of some examples of macrophages throughout the body and their specific names which you may recognize!
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Innate Immune Cells
There are various innate immune cells which are present in order to initiate a quick, constantly active immune response. These innate immune cells can be characterized whether they contain cytoplasmic granules or not, termed granulocytes or agranulocytes.
I. Granulocytes
There are 4 main cells that can be characterized as granulocytes: neutrophils, eosinophils, basophils and mast cells. Neutrophils are the most abundant immune cell which constantly circulates and primarily acts as phagocytes.
Eosinophils are primarily characterized as granulocytes associated with eradicating parasitic infections and allergies. Basophils and mast cells are very similar as their granules contain histamine which allows for increased vascular permeability and vasodilation.
II. Agranulocytes
Conversely, natural killer cells, macrophages, and dendritic cells are characterized as agranulocytes due to their lack of cytoplasmic granules.
Natural killer cells recognize a downregulation of MHC molecules which indicates viral infection — they then insert perforin and release granzyme B which initiates cell death.
Macrophages are the resident phagocytes which reside in various tissues throughout the body to uptake pathogens and present them to T helper cells. Finally, dendritic cells are known as the bridger cells between the innate and adaptive immune system.
B. Adaptive Immune Cells
There are 2 main adaptive immune cells: T and B cell lymphocytes — recall that adaptive immune system is your more specialized immune response as it can select for lymphocytes with specific receptors for a particular pathogenic antigen.
I. T Cell Lymphocytes
Finishing up maturation in the thymus, T cell lymphocytes can be divided into 2 main types: CD8+ cytotoxic T cells and CD4+ helper T cells. CD8+ T cells recognize pathogenic antigens presented on MHC-I molecules — they then kill infected/cancerous cells via the same mechanism as natural killer cells.
CD4+ T cells recognize pathogenic antigens presented on MHC-II molecules via macrophages. These cells are involved in indirect cell mediated killing by releasing pro-inflammatory cytokines which eventually results in cell death.
II. B Cell Lymphocytes
Conversely, B cell lymphocytes complete their entire maturation in the bone marrow and have a main role of producing antibodies. Once stimulated by their respective antigen, the B cell differentiates into a memory B cell for a secondary immune response and a plasma cell which constantly produces and secretes antibodies!
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
Complete the statement.
During viral infection, a __________ of MHC-I molecules allows for the activation of ____________ cells and results in the release of ___________.
A. Upregulation, Natural Killer Cells, Pro-inflammatory Cytokines
B. Upregulation, Natural Killer Cells, Perforin
C. Downregulation, Natural Killer Cells, Granzyme B
D. Downregulation, CD8+ Cytotoxic T Cells, Granzyme B
Ans. C. Downregulation, Natural Killer Cells, Granzyme B
Recall that the downregulation of MHC-I molecules indicates that there is viral infection present. Natural killer cells sense this lack of MHC-1 expression and allow for the insertion of perforin and granzyme B.
Sample Practice Question 2
When looking at a blood smear for a possible case of blood cancer, the pathologist notices an abundant amount of cells which look to have abundant phagocytic ability and no presence of cytoplasmic granules. Which of these cells can be possibly cancerous based off of the description?
I. Macrophages
II. Neutrophils
III. Dendritic Cells
A. II only
B. III only
C. II and III
D. I and III
Ans. D. I and III
Because the cell in question has no cytoplasmic granules, we can eliminate neutrophils as those are characterized as granulocytes. Macrophages and dendritic cells both do have phagocytic capacity and are characterized as agranulocytes because they have no cytoplasmic granules.


 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these