I. What are the Various Endocrine Regulations of the Skeletal System?
You might have read the title of this article and maybe got surprised: how could these 2 different organ systems be related? One system is meant for giving our body a protective foundation while the other primarily regulates metabolic and physiological homeostasis.
However, when we get past the superficialities, we see that there’s an important interconnection between these 2 systems which is crucial in helping us maintain calcium homeostasis! To understand this a little bit better, we’ll have to kick it a little bit back to endocrine basics — let’s get started!
II. The Role of the Skeletal System in Calcium Homeostasis
Recall that bone is a type of connective tissue because it contains a ground substance which acts as the gel matrix which contains various cells and fibers. Important cells include osteoblasts and osteoclasts which we’ll come back to later on while the main embedded fibers include collagen and elastic fibers.
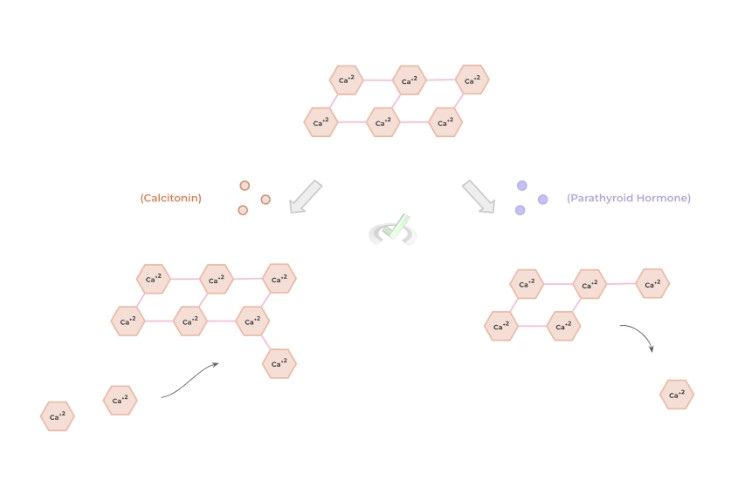
In this case, the ground substance of bone is composed of hydroxyapatite crystals, which are composed of calcium and phosphate and written as Ca₁₀(PO₄)₆(OH)₂. Don’t worry about memorizing this: the most important thing to know is that this is the source of calcium within the bone!
A. Mechanism of Action of Calcitonin
As with many of the ions within our bloodstream, there needs to be a delicate balance of calcium levels within the blood in order to maintain homeostasis. In circumstances where blood calcium is TOO HIGH, the release of calcitonin by the C cells located in the thyroid gland occurs!
Calcitonin works by allowing for increased bone deposition which is basically a fancy term referring to the formation of new bone tissue! In this case, calcitonin allows for the activation of osteoblasts which allows for the deposition of the bone matrix crystals and fibers.
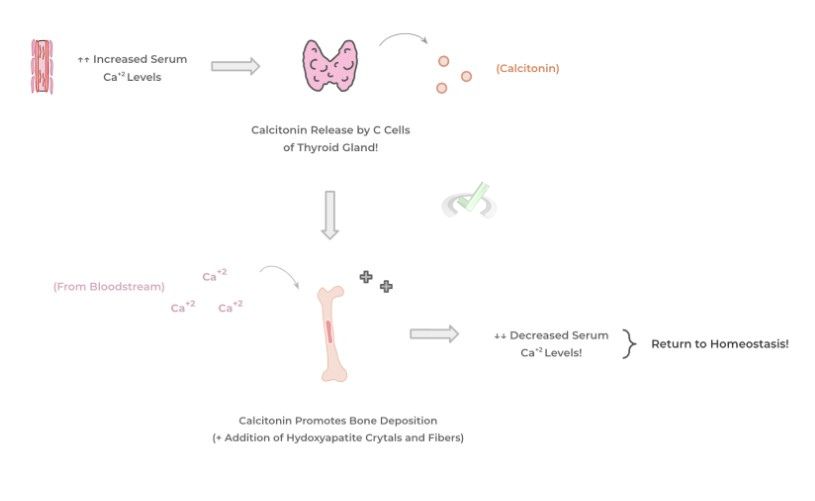
In this case, the source of calcium from the crystals comes from the increased serum calcium concentration! Thus, by increasing bone deposition, the blood serum calcium can be uptaken into the bone and decreased in order to return to homeostasis!
Finally as seen in many pathways in the human body, there’s always a negative feedback loop in place in order to suppress the pathway from pursuing despite physiological homeostasis being established!
B. Mechanism of Action of the Parathyroid Hormone (PTH)
What if we go the opposite way and the serum calcium DECREASES? In this case, the main player in returning Ca+2 concentrations back to normal is the parathyroid hormone (PTH) which is released by the parathyroid glands, which are 4 pea sized glands located in the back of the thyroid!
In this case, PTH works by increasing bone resorption which again is another fancy word for the breakdown of bone tissue. The main cells stimulated for this are osteoclasts which work to create an acidic and proteolytic environment to promote the breakdown of bone tissue!
Through this, the release of calcium from the hydroxyapatite crystals occurs in order to allow for an increase in blood serum calcium, returning the levels back to physiological homeostasis!
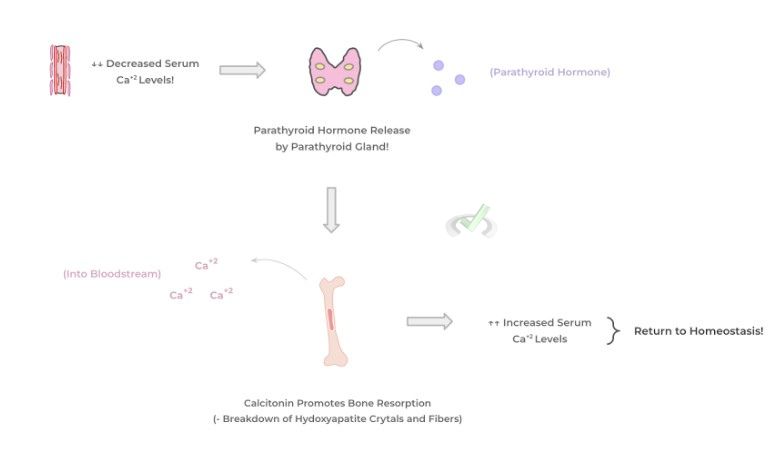
As shown above, the delicate interplay of these two hormones is important in order to maintain proper calcium levels within the blood and throughout the entire body! Look below down below again for a summarized visual diagram concerning the actions of calcitonin and PTH!
III. Bridge/Overlap
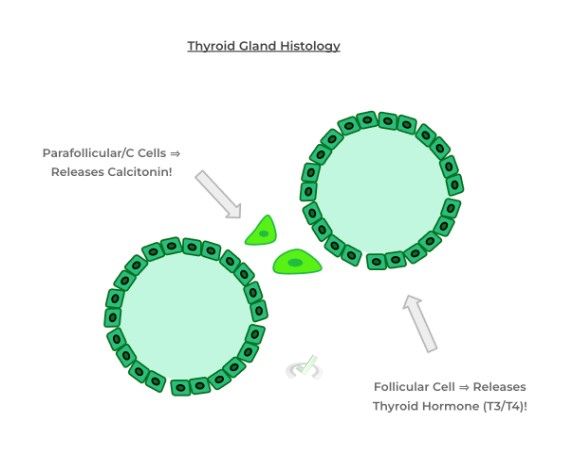
It’s definitely notable that the thyroid gland secretes many different types of hormones that it can be hard to keep track of! Let’s go ahead and review the 2 basic hormones secreted by the thyroid gland in order to differentiate them and prevent any misconceptions or misunderstandings!
I. Follicular Cells v.s. Parafollicular/C Cells of the Thyroid Gland!
As we mentioned above, the thyroid gland is responsible for the release of 2 main hormones: the thyroid hormone (T3/T4) and calcitonin which work to increase metabolic activity and decrease blood serum calcium levels, respectively.
It’s important to note that the thyroid hormone is released by the follicular cells of the thyroid gland as shown below. Conversely, calcitonin is released by the C cells of the thyroid gland — these are also called the parafollicular cells of the thyroid gland because they lie in between the thyroid follicles as shown below.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Mechanism of Action of Calcitonin
In response to high blood serum calcium, calcitonin will be released by the follicular cells of the thyroid gland! This then allows for increased bone deposition via increased activation of the osteoblasts of the bone tissue!
This allows for increased formation of bone tissue where the calcium needed to form the hydroxyapatite crystal bone matrix comes from the blood! This then results in a lowering of blood serum calcium allowing for a return to homeostasis.
B. Mechanism of Action of the Parathyroid Hormone
Conversely in response to low blood serum calcium, the parathyroid hormone will be released from the parafollicular cells of the parathyroid gland. This then allows for increased bone resorption via the activation of osteoclasts of the bone tissue.
In this case, this creates a proteolytic and acidic environment within the bone tissue which allows for bone breaking down — this then allows for the release of calcium into the bloodstream which increases blood serum calcium!
V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
Chronic hyperparathyroidism is a condition characterized by hyperactivity of the cells of the parathyroid glands. Which of the following physiological effects would result from this condition?
A. Increased Bone Density
B. Increased Bone Deposition
C. Decreased Serum Calcium
D. Decreased Bone Density
Ans. D
Chronic hyperparathyroidism would result in an increased release of PTH without responding to negative feedback. As such, this would result in increased bone resorption, decreased bone density, and increased serum calcium levels!
Sample Practice Question 2
Denosumab is a type of medication utilized for the treatment of osteoporosis which is a chronic condition characterized by the progressive weakening of bone tissue. Based on this, which of the following is the most likely mechanism of action?
A. Calcitonin Antagonist
B. Parathyroid Hormone Agonist
C. Osteoblast Inhibitor
D. Osteoclast Inhibitor
Ans. D
In this case, we’re trying to prevent further bone breakdown and increase the formation of bone tissue! An osteoclast inhibitor would prevent bone resorption which would prevent bone breakdown!
A calcitonin antagonist would be non beneficial because we would decrease bone tissue formation. Likewise, a PTH agonist would further promote bone breakdown. Finally, inhibition of the osteoblasts would also prevent new bone tissue from forming!


 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these