I. What are the Breathing Mechanisms and Regulations of the Respiratory System?
Try and follow this breathing exercise: Close your eyes. Inhale and take a deep breath for 4 seconds, hold your breath for 4 seconds, exhale for 4 seconds, and finally hold for 4 seconds. This is called box breathing and is a great way for you to relax and reach a calm state in many situations such as before a test, before sleeping, etc.
While we usually think of breathing as a generally passive action that we do unconsciously (which is true), there are definitely components of muscular and nervous system control that are actively involved in getting O2 into our system and getting CO2 out. Let’s go ahead and get a better insight of how we breathe and what regulatory measurements are taken to control our breathing.
II. Mechanisms of Breathing and Regulation
As mentioned above, the passive process of breathing is governed by a wide range of interplay between nervous and muscular components. Additionally, there are various physiological regulators which can control our breathing rate because recall that how fast we breathe can also have an effect on our physiological pH.
A. Mechanism of Breathing
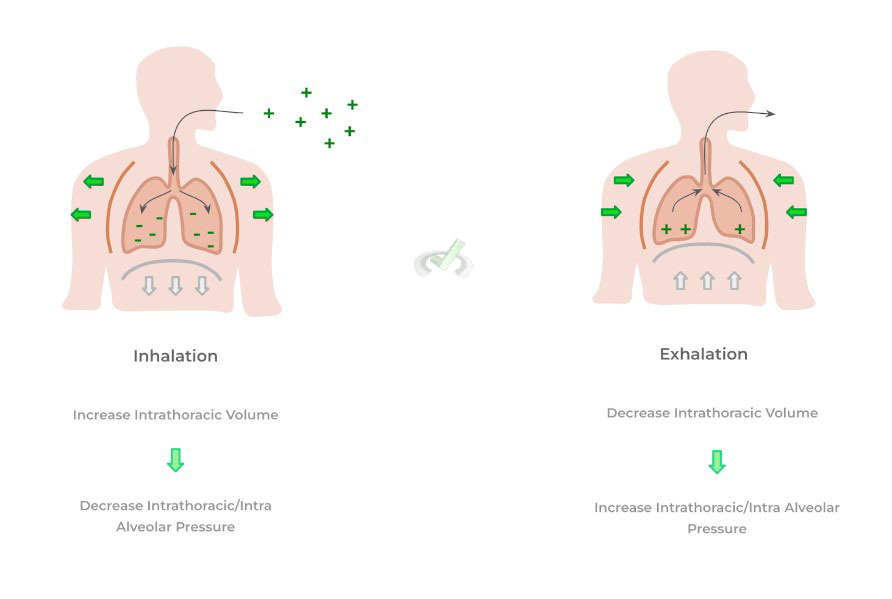
As you all have experienced, breathing can be divided into 2 main stages: inhalation and exhalation. The main driving forces which allow for breathing to occur include changes in intrathoracic volume and pressure — these are basically changes in the chest cavity volume and pressure essentially!
I. Inhalation
The main driver of inhalation is the contraction of the diaphragm: in its relaxed state, the diaphragm pushes up against the lung which decreases the intrathoracic volume. Contraction of the diaphragm pulls this muscle down which now prevents it pushing up against the lung — as a result, there’s an increase in intrathoracic volume!
Due to Boyle’s law, the increase in intrathoracic volume results in a corresponding decrease in intrathoracic pressure — and thus, a decrease in intra alveolar pressure.
Additionally, because air wants to move from a region of high pressure to low pressure, air outside of the body (which is at a higher, atmospheric pressure) flows into the lungs because of the lower intrathoracic pressure generated via chest cavity expansion!
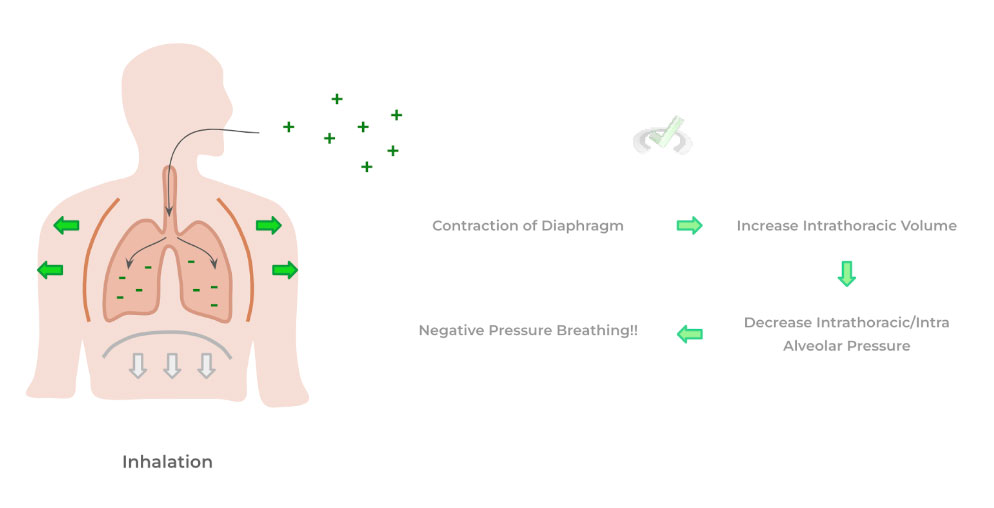
This process of breathing is actually called negative pressure breathing because of the negative pressure gradient generated by the decreased intrathoracic pressure which in turn was generated by the expansion of the chest wall cavity.
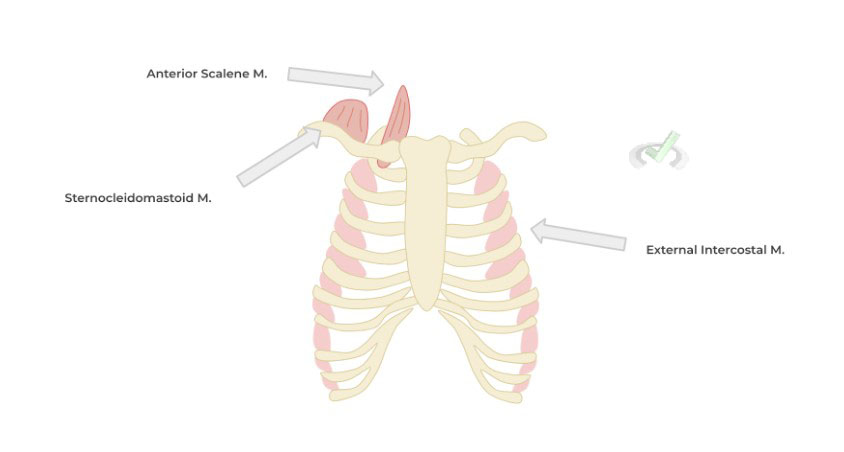
In cases where extra effort is required to inhale air into the lungs, accessory respiratory muscles are recruited in order to further maximize the expansion of the chest cavity. As shown above, these include muscles such as the external intercostal muscles, the scalene muscles, and the sternocleidomastoid muscle!
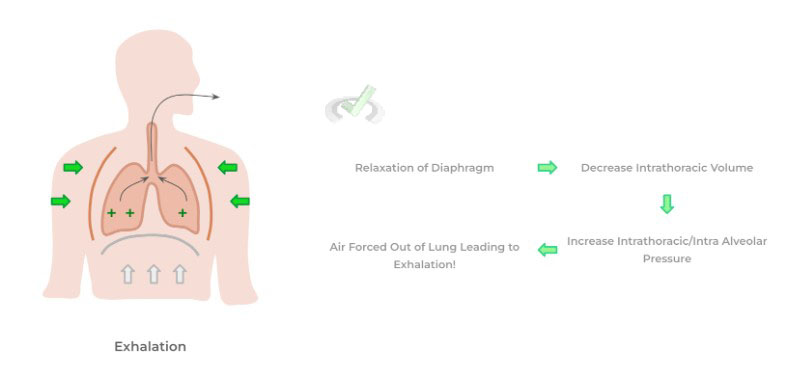
II. Exhalation
Conversely, the main driving force which allows for exhalation is the relaxation of the diaphragm: this results in the muscle pushing back up agains the lungs which decreases their intrathoracic volume.
Again, via Boyle’s law, the decrease in chest cavity volume results in an increase of intrathoracic/intra alveolar pressure which forces air of the lung into the environment which completes the process of exhalation.
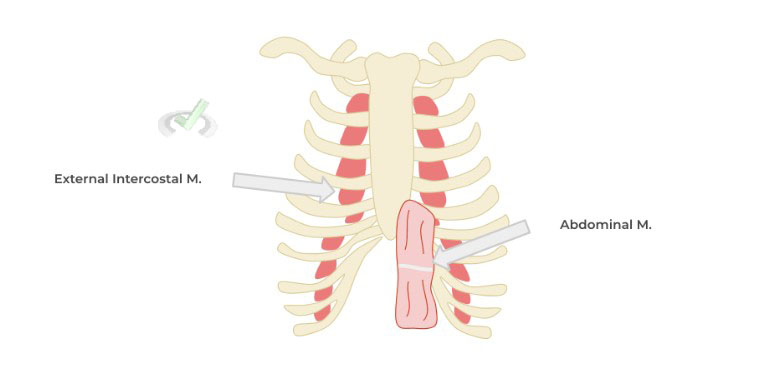
In a similar way, additional accessory respiratory muscles can also be recruited in order to further decrease the volume of the chest cavity in cases where an individual needs to forcefully expire — these muscles include the abdominal muscles as well as the internal intercostal muscles!
B. Regulation of Breathing
While breathing is an unconscious, autonomic process, there are various physiological changes which have the ability to regulate the action of breathing. Within the nervous system, particularly the medulla oblongata of the brainstem, there are various clusters of cells which work to regulate breathing rate called respiratory control centers.
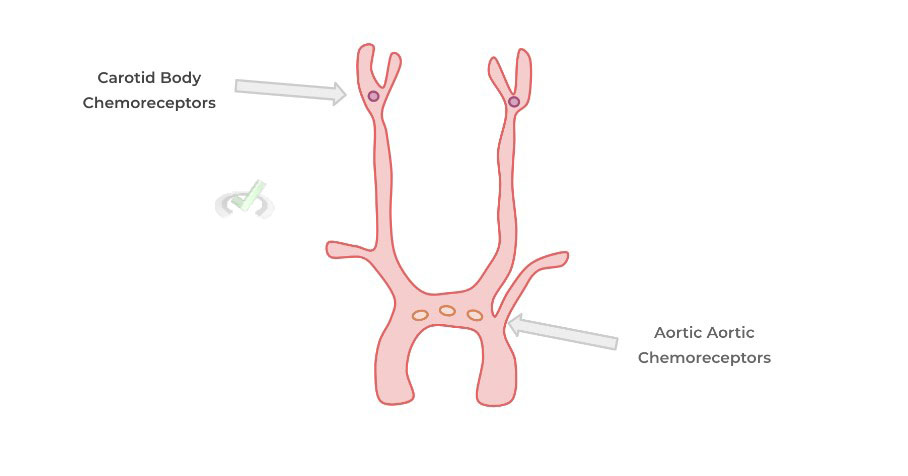
These work by integrating incoming signals from the body which sense physiological changes — based on the physiological changes identified, the respiratory response centers adjust the breathing rate accordingly. The best example would be in regards to changes in the physiological blood pH as it needs to be maintained in a narrow range — these changes in blood pH are constantly sensed via chemoreceptors located in within the carotid bodies and aortic arch!
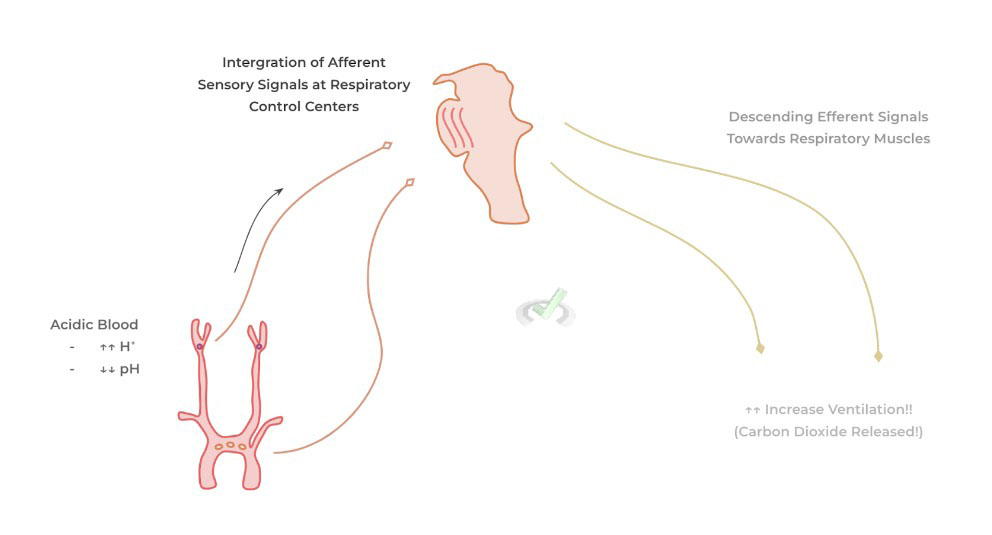
If blood pH becomes to acidic (increased H+/decreased pH), the carotid body and aortic arch chemoreceptors sense this physiological change and send afferent, sensory impulses to the respiratory control centers.
The respiratory control centers then send efferent, motor impulses which stimulate the various nerves associated with breathing to INCREASE VENTILATION in order to exhale more CO₂ in an effort to decrease the acidity!
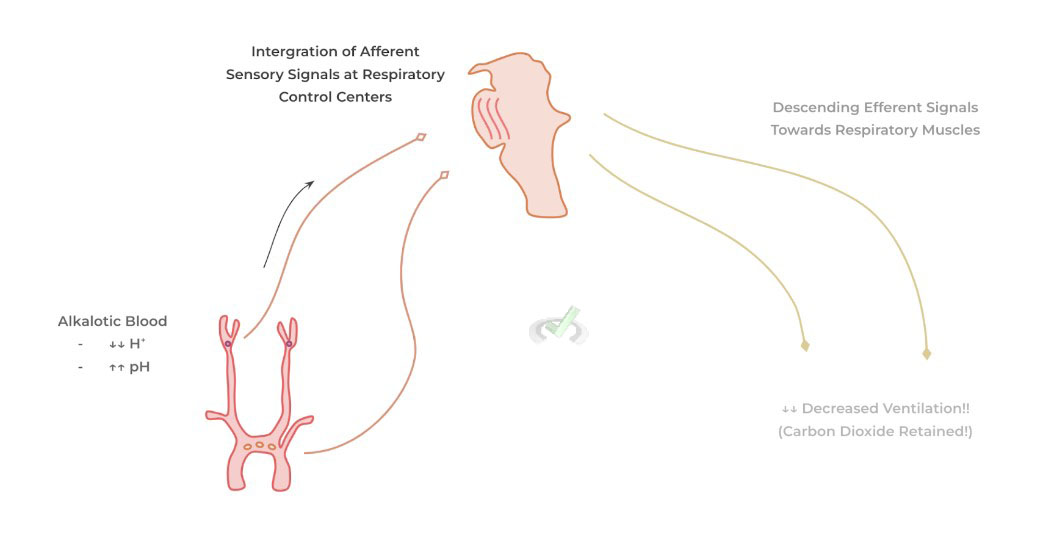
If blood pH becomes to alkalotic (decreased H+/increased pH), the carotid body and aortic arch chemoreceptors sense this physiological change and there’s a similar relaying of afferent sensory signals, integration at the level of the respiratory control centers, and exit of efferent motor signals to the respiratory muscles in order to DECREASE VENTILATION in order to retain more CO₂.
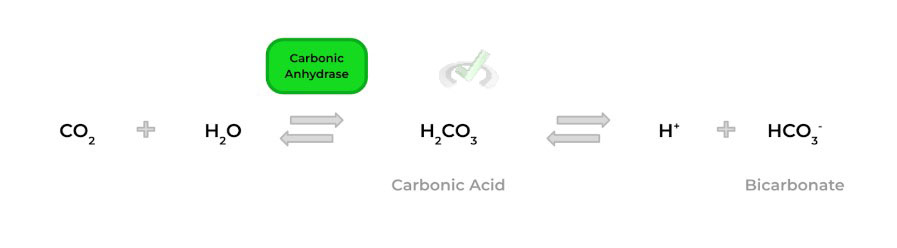
Recall that the concentration of carbon dioxide within the blood is a main determinant in regards to the acidity/alkality of the blood — this is due to the set of chemical reactions where carbon dioxide and water can combine to form carbonic acid, which can then dissociated to form protons (H+).
III. Bridge/Overlap
As we mentioned above, Boyle’s law is a key principle in general chemistry which helps to explain how breathing occurs in the context of increasing/decreasing intrathoracic/chest cavity volume. Let’s go ahead and draw up a quick review of Boyle’s Law!
I. Boyle’s Law
Recall that Boyle’s Law states that in states of constant moles of gas and temperature, the pressure and volume of a gas are inversely/indirectly proportional to one another! Additionally, recall how Boyle’s Law (and all the other ideal gas laws) are derived from the ideal gas equation.
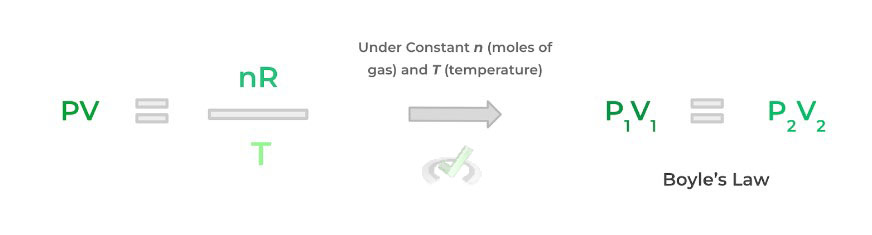
Inhalation and exhalation are a great represent of Boyle’s law from a physiological perspective! Inhalation is driven by an increase in intrathoracic volume and because of Boyle’s law there’s an inverse decrease in intrathoracic pressure driving negative pressure breathing. Conversely, exhlation is driven by a decrease in intrathoracic volume and an increase in intrathoracic pressure driving the flow of air out.
IV. Wrap Up/Key Terms
Let’s take this time to wrap up & concisely summarize what we covered above in the article!
A. Mechanism of Breathing
Breathing can actually be thought of as a physiological application of Boyle’s law, where changes in intrathoracic volume result in changes in intrathoracic pressure which drive the process of breathing.
I. Inhalation
The main driver of inhalation is the contraction of the diaphragm which pulls the muscle down allowing for expansion of the thoracic cavity. This increase in chest cavity volume results in a decrease in intrathoracic/intra alveolar pressure which allows for air to flow from the outside (with a greater air pressure) to the lower air pressure within the lungs, a process called negative pressure breathing.
In addition, in cases where effort is required in order to inhale air such as in the case of lung disease, accessory respiratory muscles such as the anterior scalene, the sternocleidomastoid, and the external intercostal muscles can be recruited in order to further increase the volume of the chest cavity.
II. Exhalation
The main driver of exhalation is the relaxation of the diaphragm which allows the muscle to push back up the chest cavity and decrease intrathoracic volume. This results in an increase in intrathoracic/intra alveolar pressure resulting in air to flow out of the lungs.
Similarly, accessory respiratory muscles such as the abdominal and internal intercostal muscles can also be recruited in order to further decrease the volume of the chest cavity to promote exhalation.
B. Regulation of Breathing
The main regulatory physiological stimulus that can result in a change of breathing rate/ventilation is blood pH. Changes in blood pH are sensed by specialized chemoreceptors located in the carotid bodies and the aortic arch. These send afferent, sensory signals to respiratory control centers within the medulla oblongata which then sends efferent motor signals to the respiratory muscles to adjust breathing adequately.
If the pH of the blood becomes acidic, then the chemoreceptors send afferent signals to the respiratory control centers which send efferent signals to the respiratory muscle to INCREASE THE BREATHING RATE (i.e. hyperventilate). If the pH of the blood become alkalotic, a similar cascade of signaling occurs but ultimately results in DECREASING THE BREATHING RATE (i.e. hypoventilation).V. Practice
Take a look at these practice questions to see and solidify your understanding!
Sample Practice Question 1
Complete the following statement.
Based on the physiological application of Boyle’s law to breathing, a ____________ in intrathoracic volume results in a _______________ in intrathoracic/intra alveolar pressure. This process is known as _____________.
A. Increase, Increase, Exhalation
B. Decrease, Decrease, Inhalation
C. Decrease, Increase, Inhalation
D. Decrease, Increase, Exhalation
Answer: D. Decrease, Increase, Exhalation
This statement is the only one which has the correct usage of the terms. Exhalation results from the relaxation of the diaphragm which decrease intrathoracic volume and thus increases intrathoracic/intra alveolar pressure.
Sample Practice Question 2
Suppose a patient’s body is in a diseased state where there’s an increase in lactic acid fermenation in metabolims. Which of the following correctly describes what the chemoreceptors at the carotid bodies and aortic arch would sense and the appropriate change in breathing rate?
A. Increased pH, Hyperventilation
B. Decrease pH, Hypoventilation
C. Decreased pH, Hyperventilation
D. Increased pH, Hypoventilation
Answer: C. Decreased pH, Hyperventilation
Because there’s an increase in lactic acid fermentation, the blood will be in an acidic state and will result in a decreased pH. As a result, the appropriate change in the breathing rate is to increase ventilation (i.e. hyperventilate) in ordert to exhale carbon dioxide in order to decrease the acidity.



 To help you achieve your goal MCAT score, we take turns hosting these
To help you achieve your goal MCAT score, we take turns hosting these 

 reviews on TrustPilot
reviews on TrustPilot